Understanding Psoriasis: A Comprehensive Guide
Table of Contents
Understanding Psoriasis: A Comprehensive Guide
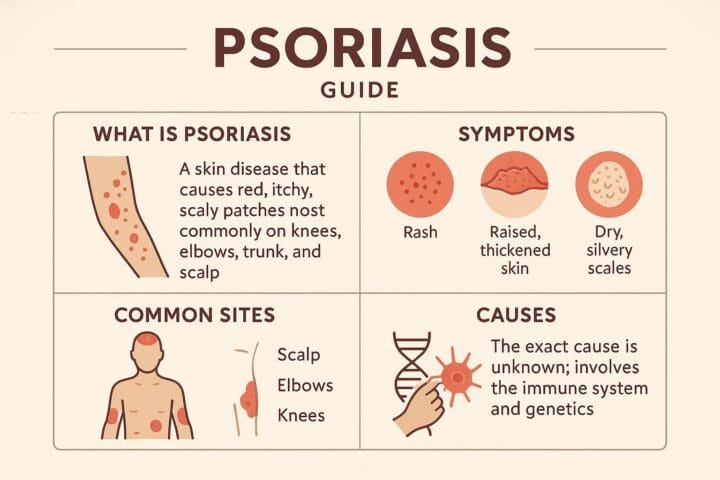
Psoriasis is a chronic autoimmune condition affecting approximately 7.5 million adults in the United States, characterized by an accelerated skin cell growth cycle. Instead of the typical month-long cycle, skin cells in individuals with psoriasis mature in just 3 to 4 days, leading to a buildup of thick, scaly plaques on the skin’s surface. These plaques can be dry, raised, inflamed, itchy, uncomfortable, and sometimes painful. The condition is not contagious and affects males and females equally, with peak onset ages between 15-25 and 50-60 years old.
Understanding Psoriasis: Types and Characteristics
Plaque Psoriasis Lesions
Plaque psoriasis lesions, the most common type of psoriasis, exhibit several distinct characteristics:
- Appearance: Plaque psoriasis lesions are typically raised patches of thickened skin, often described as plaques, which can be small papules (small, raised bumps) or larger lesions bigger than a thumbnail. They are well-demarcated, meaning they have distinct borders.
- Coloration: The color of the plaques can vary depending on skin tone. On lighter skin, they often appear red or pink with silvery-white scales. On light brown skin, they may be salmon-colored with silvery scales. For individuals with darker skin, the plaques can range from brown, purple, or gray with grey scales, and the redness may be less pronounced or harder to see.
- Scaling: A hallmark of plaque psoriasis is the presence of overlying scales. These scales are typically silvery-white, dry, and thick, resulting from the rapid overproduction of epidermal cells. The scales can shed easily, but those beneath tend to stick together. If scratched, the scales may tear away, potentially causing bleeding.
- Texture and Thickness: The plaques are thick and rough to the touch. They can be slightly elevated above the skin surface.
- Symptoms: Plaque psoriasis lesions can cause significant itching, especially during flares and when affecting the scalp. Pain can also occur, particularly when the plaques are thickened and cracked, such as on the palms and soles. Other symptoms include irritation, burning, and stinging sensations.
- Location: Plaque psoriasis can appear anywhere on the body, but commonly affects extensor surfaces like the elbows and knees, as well as the scalp, trunk, lower back, and gluteal fold. They can also be found on the face (hairline, forehead, eyebrows, eyelids, ear canals, behind the ears), flexural areas (skin folds), genitals, palms, soles, and nails.
- Symmetry: The plaques are often symmetrical, meaning if they appear on one side of the body (e.g., one elbow), they are likely to appear on the other.
- Size and Coalescence: Lesions can range from a few millimeters to several centimeters in diameter. Smaller plaques can coalesce to form larger ones, potentially involving extensive areas of the skin, especially on the trunk and limbs.
- Auspitz Sign: Upon removal of the silvery-white scales, pinpoint bleeding spots may be observed, a clinical sign known as Auspitz sign.
- Koebner Phenomenon: The presence of isomorphic lesions (similar lesions) along the line of trauma indicates active disease and is known as the Koebner phenomenon.
- Variations in Specific Body Areas:
- Scalp: Lesions can range from fine scaling to thick, crusted plaques covering the entire scalp.
- Flexural Areas: In moist environments like skin folds, plaques are well-defined red patches that may lack typical scales and can be misdiagnosed as fungal infections.
- Genital Area: These lesions appear as bright red, shiny patches without scales.
- Palms and Soles: Characterized by thick, scaly plaques with painful fissures.
- Nails: Psoriasis can affect fingernails and toenails, causing pitting, onycholysis (nail separation), ridging, and dystrophy.
- Chronic and Relapsing Nature: Plaque psoriasis is a chronic, relapsing, and remitting condition, meaning it can flare up unexpectedly and then subside. There is no cure, but treatments can help manage symptoms.
Guttate Psoriasis Spots on a Torso
Guttate psoriasis spots on the torso exhibit several distinct characteristics:
- Appearance and Shape: The spots are typically small, round, or teardrop-shaped, resembling raindrops that have fallen over the body. The term “guttate” itself comes from the Latin word for “drop.”
- Size: These lesions usually range from 2 to 10 millimeters (mm) in width, or about 0.5 to 1.5 centimeters in diameter. They are generally smaller than the plaques seen in plaque psoriasis.
- Coloration: The color of the spots can vary depending on skin tone. On lighter skin, they appear pink or red. On darker skin tones, the patches may be purple, violet, brown, or dark brown, and the redness may be harder to discern.
- Scaling: Guttate psoriasis spots are often covered by a fine, dry, white, or white-grey scale. This scale can be subtle in early lesions. Unlike plaque psoriasis, the scales are not as thick.
- Distribution: While they can appear almost anywhere on the body, guttate psoriasis lesions are predominantly found on the torso, as well as the arms and legs. They tend to be widespread and numerous, with the number of lesions ranging from 5 to over 100.
- Distinctness: Each patch is usually distinct and surrounded by healthy skin.
- Symptoms: The patches are often irritated and can be itchy, burning, or sore.
- Onset: Guttate psoriasis typically has an acute onset, developing over a few days. It often appears suddenly, usually following an infection.
- Triggers: A common trigger for guttate psoriasis is a bacterial infection, most frequently a streptococcal infection of the upper respiratory tract, such as strep throat. Other triggers can include other viral infections (like SARS-CoV-2 or coxsackievirus), certain medications, skin injury, and stress.
- Duration and Progression: In most cases, an outbreak of guttate psoriasis lasts two to three weeks and the spots tend to clear up on their own, often within a few weeks to months. However, about one-third of individuals who experience guttate psoriasis may go on to develop a more chronic form of psoriasis, such as plaque psoriasis.
- Demographics: Guttate psoriasis is more common in children and young adults, typically under 30 years old, and is the second most common form of psoriasis in children after chronic plaque psoriasis.
Common Discolorations of Nail Psoriasis
Nail psoriasis, an autoimmune condition, leads to various discolorations in both fingernails and toenails due to the immune system’s overreaction, causing rapid skin cell growth. These discolorations are a common symptom, affecting the skin underneath the nails, known as the nail bed.
Here are common discolorations associated with nail psoriasis:
- Salmon Patches or Oil Drop Spots: These appear as yellowish-red patches under the nail plate, resembling a drop of oil. The yellow color is attributed to parakeratotic and acanthotic processes occurring beneath the nail, while reddish tones are due to plaque on the nail bed.
- Yellow, Red, Pink, or Brown Discoloration: The nail bed can generally change to these colors.
- White Patches (Leukonychia): White discoloration can occur on the nails. Crumbling nails often turn white.
- Redness in the Lunula: The lunula, the half-moon shape at the base of the nail, may appear red due to dilated blood vessels, indicating a more severe case of psoriasis.
- Splinter Hemorrhages: These are small, dark-red or reddish-purple lines that run from the tip of the nail to the cuticle, caused by burst blood vessels.
- Yellow-Brown Discoloration: The entire toenail or fingernail can turn a yellow-brown color.
- White or Yellowish Patch with Onycholysis: When the nail separates from the nail bed (onycholysis), a white or yellowish patch typically appears at the tip of the nail and can extend down to the cuticle.
- Dark Coloration from Infection: If bacteria enter the space created by onycholysis, the entire nail can turn a dark color.
- White-to-Gray Coloring: In cases of nail bed hyperkeratosis, where cells accumulate under the nail plate, patients may present with white-to-gray coloring, in addition to yellow and oily nails.
- Variations in Color with Thickening: The overproduction of keratinocytes in nail psoriasis can lead to thickening, malformation, and discoloration of the nails.
Types of Psoriasis
Psoriasis manifests in several forms, and individuals can experience more than one type simultaneously or throughout their lifetime:
- Plaque Psoriasis: The most common type, affecting 80-90% of people with psoriasis. It presents as raised, red patches covered with silvery scales, often appearing on the trunk, buttocks, scalp, and extremities. On darker skin tones, plaques may appear darker, thicker, purple, grayish, or dark brown.
- Inverse Psoriasis: This type develops in skin folds, such as under the breasts, in the armpits, genital area, and buttocks. It causes smooth, deep-red or darkened, inflamed skin without scales and can be severely itchy and painful, worsened by sweat and rubbing.
- Guttate Psoriasis: Occurs in less than 30% of people with psoriasis and often appears after a streptococcal infection (like strep throat). It manifests as small, red, drop-shaped scaly spots, commonly affecting children and young adults on the arms, legs, and torso.
- Pustular Psoriasis: A rare form characterized by white pustules (blisters of pus) surrounded by inflamed skin. These pustules can appear on specific areas like hands and feet or cover most of the body. Generalized pustular psoriasis (GPP) is a difficult-to-treat type, with spesolimab (an IL-36 inhibitor) being the only FDA-approved treatment for it.
- Erythrodermic Psoriasis: A severe and rare type affecting 1-2.25% of people with psoriasis, causing widespread redness, scaling, and peeling of the skin.
Understanding Psoriasis: Unpacking the Causes and Common Triggers
Psoriasis is a chronic autoimmune condition that primarily affects the skin, leading to thick, discolored patches covered with scales. While not contagious, it can significantly impact a person’s quality of life. Understanding the underlying causes and identifying common triggers are crucial steps in managing this condition.
The Root Causes of Psoriasis
The exact reasons why psoriasis develops are not fully known, but research points to a complex interplay between the immune system and genetics.
- Immune System Dysfunction: In individuals with psoriasis, the immune system mistakenly identifies healthy skin cells as foreign invaders. Specifically, white blood cells called T-cells, which normally fight off harmful bacteria and viruses, begin to attack healthy skin cells. This errant attack leads to an accelerated production of new skin cells. Normally, skin cells take about 3 to 4 weeks to mature and shed; however, in people with psoriasis, this process is dramatically sped up to just 3 to 7 days. This rapid turnover results in the accumulation of immature cells on the skin’s surface, forming the characteristic flaky, crusty patches and scales.
- Genetic Predisposition: Psoriasis often runs in families, indicating a strong genetic component. While many different genes have been linked to the development of psoriasis, having these genes doesn’t guarantee that a person will develop the condition. It is believed that certain gene combinations may increase vulnerability. It’s also possible to develop psoriasis even without a family history of the disease.
Common Triggers for Psoriasis Flares
While the immune system and genetics lay the groundwork, various external and internal factors can act as “triggers,” causing psoriasis symptoms to appear for the first first time or leading to flare-ups in those already living with the condition. Triggers can vary significantly from person to person.
Here are some of the most common triggers:
- Stress: Emotional stress is a significant and very common trigger for psoriasis. The relationship can be cyclical: stress can cause a flare, and a flare can, in turn, cause more stress. Managing stress through relaxation techniques can be beneficial.
- Infections: Infections can significantly impact the immune system and are frequent triggers for psoriasis. A psoriasis flare may occur 2–6 weeks after an infection.
- Strep Throat: Streptococcal throat infections are particularly linked to guttate psoriasis, a type that often appears as small, red, drop-shaped scaly spots and frequently affects children and young adults.
- Other infections like respiratory infections, bronchitis, tonsillitis, and ear infections can also trigger flares.
- Skin Injury (Koebner Phenomenon): Psoriasis can develop in areas of the skin that have been injured or harmed. This is known as the Koebner response or phenomenon and can be caused by cuts, scrapes, insect bites, sunburns, or even vaccinations.
- Certain Medications: Some medications are known to trigger or worsen psoriasis. These include lithium, some antimalarial medicines, anti-inflammatory drugs (like ibuprofen), ACE inhibitors (for high blood pressure), prednisone, and hydroxychloroquine.
- Weather: Environmental factors like weather can play a role. Cold, dry weather can often exacerbate psoriasis flares due to less sunlight and humidity, and drier indoor air. Conversely, warm weather and natural sunlight can sometimes improve psoriasis symptoms.
- Alcohol and Smoking: Excessive alcohol consumption and smoking are both recognized as potential triggers for psoriasis flares.
- Hormonal Changes: Fluctuations in hormones, particularly in women during puberty and menopause, can trigger psoriasis.
- Weight Gain: Obesity is another factor that can trigger psoriasis symptoms.
Identifying and avoiding individual triggers is a key strategy in managing psoriasis and reducing the frequency and severity of flare-ups. If you suspect you have psoriasis or are struggling to manage your triggers, consulting a healthcare professional is recommended for personalized advice and treatment options.
Treatment and Management
Currently, there is no cure for psoriasis, but various treatments and lifestyle modifications can help manage symptoms and reduce inflammation. Symptoms typically come and go in flare-ups, with remission periods lasting 1 to 12 months.
Medical Treatments
- Topical Treatments: These are often the first-line treatment for mild-to-moderate symptoms and are applied directly to the skin. They include corticosteroids, vitamin D analogs, retinoids, anthralin, salicylic acid, and moisturizers. Coal tar is also used for itching and lesions on the scalp, palms, and soles.
- Phototherapy (Light Therapy): Controlled exposure to ultraviolet (UV) light can decrease skin inflammation and slow skin cell production. This can involve UVB narrow band, 308-nanometer excimer laser, or PUVA (psoralen combined with UVA light). However, more than 250 PUVA sessions may increase the risk of skin cancer.
- Systemic Medications: For moderate to severe psoriasis or when other treatments are ineffective, oral or injectable medications are used. These include methotrexate, cyclosporine, biologics, oral retinoids, and oral apremilast (Otezla). Janus kinase (JAK) inhibitors are a type of systemic therapy that blocks gene transcription of certain cytokines to reduce immune system inflammation.
- Immune Therapies: Newer immune therapy medications, including biologics and small molecule inhibitors, work by blocking the immune system to prevent autoimmune reactions.
Lifestyle and Home Management
- Moisturize Regularly: Keeping skin well-moisturized is crucial to prevent dryness, flaking, and flare-ups. Products containing mineral oils like liquid paraffin and petrolatum, as well as coconut oil and aloe vera gel, can be beneficial.
- Gentle Skincare: Use mild, fragrance-free cleansers and moisturizers. Warm (not hot) baths with added oils, oatmeal, sea salt, or coal tar can soothe the skin and loosen scales.
- Stress Management: Incorporate stress-reducing activities like meditation, deep-breathing exercises, yoga, and regular physical activity. Therapy or counseling can also be helpful.
- Healthy Diet: Eating a diet rich in anti-inflammatory foods such as fruits, vegetables, whole grains, lean proteins, and omega-3 fatty acids (found in fish, flaxseeds, and walnuts) can help manage symptoms. Avoid inflammatory foods like red meat, processed foods, and sugary snacks.
- Stay Hydrated: Drinking plenty of water helps keep skin hydrated and reduces dryness and flakiness.
- Protect Skin from Sunburn and Injury: While some sun exposure can be helpful, overexposure and sunburn can worsen symptoms. Use broad-spectrum sunscreen with at least SPF 30 and wear protective clothing. Avoid tattoos, piercings, and activities that may cause skin injuries.
- Avoid Alcohol and Smoking: Quitting smoking and reducing alcohol intake can significantly improve symptoms and treatment effectiveness.
- Maintain a Healthy Weight: Obesity is linked to poorer responses to biologics, and even modest weight loss can improve psoriasis severity and increase biologic efficacy.
- Clothing Choices: Opt for loose-fitting, breathable clothing made from natural fibers like cotton to avoid skin irritation.
- Consult a Dermatologist: Regular consultation with a dermatologist specializing in psoriasis is essential for personalized care plans and to stay informed about the latest treatment developments.












Post Comment