Understanding Temporomandibular Joint Disorder (TMD)
Table of Contents
Understanding Temporomandibular Joint Disorder (TMD)
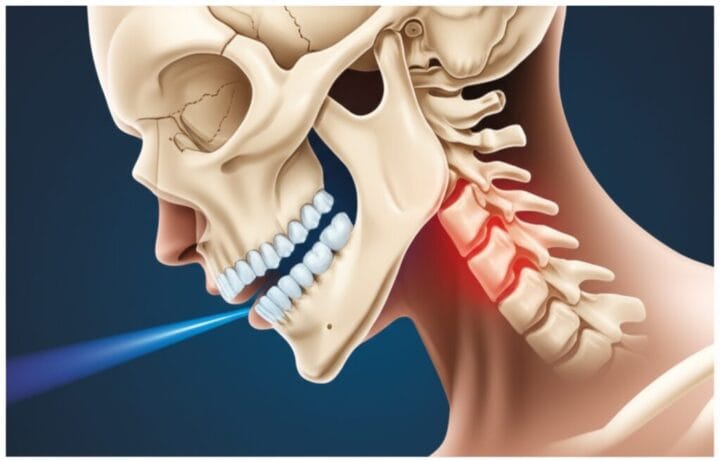
Have you ever felt a persistent click, pop, or outright pain when you chew, talk, or yawn? You might be experiencing symptoms of a Temporomandibular Joint Disorder (TMD). It’s a common issue, affecting millions of people in the U.S., particularly women between 20 and 40. Often, when people refer to “TMJ,” they are actually talking about TMD. Remember, “TMJ” is simply the name of the jaw joint itself – you have two of them, one on each side of your head – while “TMD” refers to the various conditions and disorders that can affect these joints and the muscles around them. We are talking about jaw pain, facial discomfort, headaches, earaches, and those unmistakable clicking or popping sounds that can make everyday actions surprisingly difficult. It’s frustrating to live with chronic pain that impacts your ability to eat, speak, and simply exist comfortably.
The “Aha!” Moments: A History of Jaw Understanding
Jaw troubles are far from a new phenomenon; signs of these problems appear in ancient skeletal remains, and old medical texts mention remedies for jaw pain centuries ago. Renaissance anatomists, including Leonardo da Vinci, meticulously sketched these complex joints, showcasing an early fascination with their structure. For many years, however, doctors often felt puzzled by jaw pain, sometimes dismissing it as “all in your head” due to a lack of clear understanding.
A pivotal, though now debated, moment came in the 1930s with Dr. Costen’s theory, which linked jaw pain to how a person’s teeth fit together. This idea significantly influenced dental treatments for decades. Moving forward into the 1950s and then the 1980s, healthcare finally began to take TMJ issues more seriously. Research started connecting the dots between the jaw, face, and even conditions like arthritis, leading to a more comprehensive understanding. This shift helped us see TMD not just as one simple problem, but as a complex interplay of physical, psychological, and social factors.
Understanding Jaw Troubles: Symptoms and Causes Today
When your jaw isn’t working as it should, the symptoms can range from mild annoyance to debilitating pain, significantly impacting your quality of life. Knowing what to look for can help you identify if your jaw is acting up.
The Usual Suspects: Common Symptoms of Temporomandibular Joint Disorder
- Jaw Pain or Tenderness: This is often the most common symptom. You might feel a dull ache or sharp pain in your jaw muscles, around your ear, or in your temples. It frequently worsens when you chew, talk, or yawn.
- Aching Facial Pain: Pain can spread across your face, potentially reaching your neck and shoulders, creating widespread discomfort.
- Clicking, Popping, or Grinding Sounds: Many people hear these sounds when they move their jaw. If these sounds come with pain or limit your jaw’s movement, they can be a sign of Temporomandibular Joint Disorder.
- Jaw Stiffness or Locking: Your jaw might feel stiff, especially in the morning, or even lock in an open or closed position, making it impossible to move.
- Headaches and Ear-Related Symptoms: Persistent headaches, including migraines, earaches (when there’s no infection), ringing in your ears (tinnitus), or even dizziness can all be related to TMD.
Why Your Jaw Might Be Acting Up: Common Causes of Temporomandibular Joint Disorder
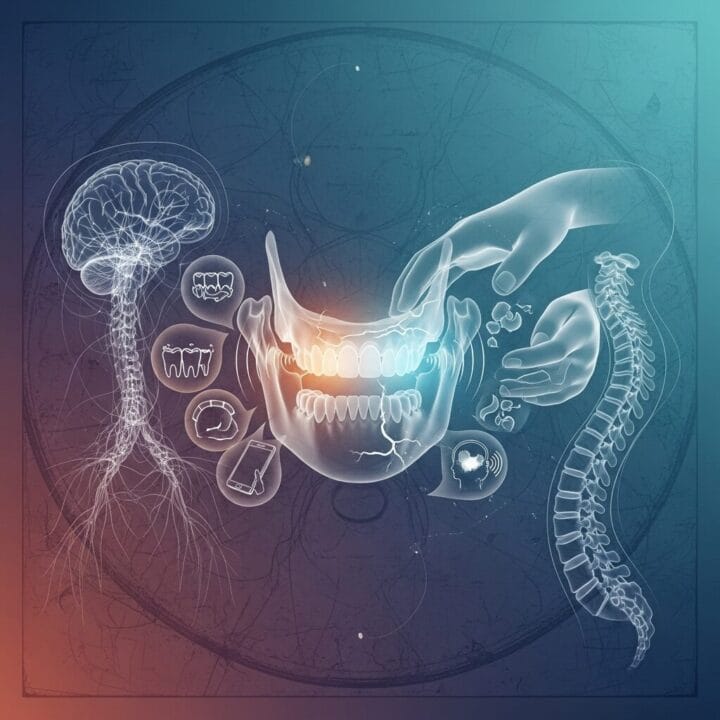
It’s rare for Temporomandibular Joint Disorder to have just one cause. Often, it’s a combination of factors that create the perfect storm in your jaw joint.
- Stress and Anxiety: When you’re stressed, you might unconsciously clench your jaw or grind your teeth, a habit known as bruxism. This puts immense strain on your jaw muscles and joints.
- Jaw Injuries: A direct blow to your face or jaw, or even whiplash from an accident, can lead to long-term TMD issues.
- Arthritis: Just like other joints in your body, your temporomandibular joints can suffer from various forms of arthritis, such as osteoarthritis or rheumatoid arthritis, causing wear and tear.
- Disk Problems: Inside your jaw joint, there’s a small, soft disk that acts as a shock absorber. If this disk erodes or slips out of its proper position, it can interfere with smooth jaw movement.
- Poor Posture: Constantly hunching over a computer or phone can strain your neck and shoulder muscles, which in turn affects your jaw posture and can contribute to TMD pain.
- Genetics: Some research suggests that your genes might play a role, making certain individuals more prone to developing Temporomandibular Joint Disorder.
Understanding these symptoms and causes is the first step toward finding relief. Do any of these sound familiar to you?
The Ongoing Debate: Differing Views on Jaw Pain
Despite our growing knowledge, certain aspects of Temporomandibular Joint Disorder remain subjects of ongoing discussion and disagreement among healthcare professionals. This complexity can make the diagnostic and treatment journey confusing for individuals seeking relief.
The Bite Battle: Is Your Bite the Blame?
Historically, a “bad bite” or malocclusion (how your upper and lower teeth meet) was frequently blamed for all jaw pain. This led to aggressive, irreversible dental work, like extensive tooth grinding or orthodontics, aimed at “correcting” the bite. Today, many experts agree that while a person’s bite might be a contributing factor, it is rarely the primary cause of Temporomandibular Joint Disorder. We now understand that permanently altering your bite to treat TMD often lacks strong scientific evidence and can even lead to more problems.
Bruxism’s Role: Cause or Symptom?
Is habitually grinding or clenching your teeth at night a direct cause of TMD, or is it another symptom of underlying stress or jaw dysfunction? The link is still debated. While bruxism certainly strains your jaw, simply noting that you grind your teeth isn’t always enough for a definitive TMD diagnosis. It’s part of a larger picture that a healthcare professional needs to evaluate.
Diagnostic Head-Scratchers: Getting a Precise Answer
Because TMD symptoms can overlap with many other health problems – from ear infections to headaches – getting a precise diagnosis can be challenging. Experts emphasize the importance of a thorough physical exam and understanding your complete medical history. They often caution against relying too heavily on expensive, unproven diagnostic gadgets that might not provide clear answers and could lead to unnecessary treatments.
Treatment Tussles: Finding the Right Approach
With no one-size-fits-all answer, Temporomandibular Joint Disorder treatment spans a wide range of approaches, leading to considerable debate.
- Conservative Versus Invasive: A significant controversy exists here. Most scientific evidence points to conservative, reversible treatments – such as self-care, simple pain relievers, and mouthguards – as the safest and most effective first steps. Invasive surgeries or permanent dental changes often lack robust evidence, carry greater risks, and can be irreversible.
- Spontaneous Improvement: Many TMD conditions improve on their own over time. This natural healing makes it difficult to definitively know if a particular treatment worked, or if the improvement was due to time, the placebo effect, or your body’s own healing mechanisms.
- The Specialist Search: Without official “TMD specialists” recognized by all medical or dental associations, finding the right doctor can be confusing. You might encounter different practitioners, each with their own philosophy and preferred treatments. This makes it crucial to seek out providers who prioritize evidence-based, conservative care.
Finding Relief: Accepted Treatments for TMD
Living with Temporomandibular Joint Disorder can be disruptive, but many effective and accepted treatments can help you manage your symptoms and improve your quality of life. We often start with the simplest, most conservative approaches.
Your First Line of Defense: Self-Care at Home!
Many people find significant relief by making simple changes at home.
- Eat Soft Foods: Give your jaw a break by choosing soft foods that don’t require heavy chewing.
- Apply Heat or Ice: Both heat and ice packs can soothe aching jaw muscles. Experiment to see which works best for you.
- Avoid Bad Habits: Try to stop chewing gum, biting your nails, or engaging in other habits that strain your jaw. Avoid excessive jaw movements like wide yawning or loud singing.
- Practice Relaxation: Pay attention to your jaw posture. Rest your tongue on the roof of your mouth, keep your teeth slightly apart, and consciously relax your jaw. Stress reduction techniques, like meditation or deep breathing, can also be very helpful.
Stepping Up: Non-Surgical Helpers
If self-care isn’t enough, your doctor or dentist might recommend other non-surgical interventions.
- Mouthguards or Splints: These custom-fit devices, worn over your teeth, can help, especially if you clench or grind your teeth at night. They stabilize your jaw joint and protect your teeth, but they should not permanently change your bite.
- Physical Therapy: A physical therapist can teach you gentle exercises to stretch and strengthen your jaw muscles and improve joint movement. Techniques like massage, ultrasound, or Transcutaneous Electrical Nerve Stimulation (TENS) might also be used to relax muscles and reduce tension.
- Medications: Over-the-counter pain relievers, such as ibuprofen, can help with mild to moderate pain. For more severe symptoms, your doctor might prescribe muscle relaxants, or even low-dose antidepressants, which can help with pain, bruxism, and sleep. In some cases, Botox injections into specific jaw muscles are used to ease chronic muscle pain.
- Mind Over Matter: Counseling, cognitive behavioral therapy (CBT), and biofeedback can be surprisingly effective. These therapies help you understand and manage chronic pain by addressing behavioral and psychological factors.
When Things Get Serious: Minimally Invasive & Surgical Options
For very stubborn cases of Temporomandibular Joint Disorder where conservative treatments haven’t provided relief, or if there is significant damage to the joint, more advanced procedures might be considered.
- Minimally Invasive Procedures:
- Arthrocentesis: This involves inserting small needles into the joint to flush out inflammatory fluid and debris.
- TMJ Arthroscopy: A tiny camera and small instruments are used to visualize and address issues inside the joint, such as removing scar tissue or repositioning the disk. It’s less invasive than open surgery and has a faster recovery.
- Open-Joint Surgery: This is a last resort for severe structural damage or persistent pain. It involves direct access to the joint and carries higher risks, so always seek a second opinion before considering this option.
Remember, the goal is always to find the least invasive yet most effective treatment that provides lasting relief from your Temporomandibular Joint Disorder symptoms.
Looking Ahead: The Future of TMD Care
The landscape of Temporomandibular Joint Disorder diagnosis and treatment is continuously evolving, with exciting advancements on the horizon. Researchers are working to develop more precise ways to understand and treat this complex condition.
Smarter Diagnostics: Pinpointing the Problem Early
- Advanced Imaging: Imagine seeing your jaw move in real-time! New 3D imaging, dynamic MRIs, and Cone Beam Computed Tomography (CBCT) are providing incredibly detailed views of the jaw joint and surrounding structures. This allows doctors to spot misalignments, joint erosion, and inflammation with unprecedented accuracy.
- AI for Early Risk Prediction: Artificial Intelligence (AI), combined with advanced scans, is being explored to detect subtle jaw differences that might indicate a higher risk for TMD before significant symptoms even appear.
- Biomarkers: Scientists are actively searching for “biomarkers”—tiny clues in your body, like proteins or genetic markers—that could help diagnose Temporomandibular Joint Disorder earlier and track how well treatments are working.
- Functional Analysis: Technologies like Condylography and Tekscan are emerging to precisely map jaw movement and analyze bite forces, giving a clearer picture of mechanical issues.
Cutting-Edge Treatments: Healing from Within
- Regenerative Medicine: The future of healing might involve your own body’s power. Therapies like Platelet-Rich Plasma (PRP) and Platelet-Rich Fibrin (PRF) use concentrated components from your blood to promote natural healing and reduce inflammation in the jaw joint. Stem cell therapy is also being investigated to repair damaged TMJ tissues for long-lasting relief.
- Targeted Drugs: We may see new medications, similar to those developed for migraines (CGRP antagonists), that specifically block pain signals related to Temporomandibular Joint Disorder, offering more focused relief.
- Bioengineered Joints: Researchers are working on groundbreaking projects, like growing new jaw joint discs in labs from rib tissue. This “sci-fi” concept could become a reality for those with severe joint damage, offering a biological replacement.
- Refined Technologies: Expect more refined laser therapy, ultrasound, and specialized 3D-printed splints that offer a perfect, customized fit and more effective symptom management.
Research Frontiers: Unraveling the Complexity
Ongoing research is delving deeper into the fundamental questions about Temporomandibular Joint Disorder:
- Genetic Puzzles: Why are some people more susceptible to TMD? Researchers are trying to unravel the genetic links that predispose individuals to the condition.
- Mind-Body Connection: The link between stress, inflammation, and jaw pain is being explored further, including how gut microbes might even play a role.
- Holistic Approaches: A greater focus on understanding the connection between your posture, neck health, and jaw pain is leading to more holistic treatment strategies.
- Patient-Centered Care: There’s an increasing emphasis on involving patients directly in research and care decisions, ensuring treatments truly meet their real-world needs and experiences.
These advancements offer hope for more personalized, effective, and less invasive treatments for Temporomandibular Joint Disorder in the years to come.
Don’t Keep Your Jaw a Secret! When to Seek Professional Help
If you’re experiencing constant jaw pain or tenderness, difficulty opening your mouth, or if your jaw frequently locks up, it’s important to get it checked out. Don’t let your discomfort linger. Talk to your dentist or doctor. They can help you find the right healthcare professional, such as a TMJ specialist or an oral surgeon, to get a proper evaluation and create a personalized plan for you. Seeking help early can make a significant difference in managing Temporomandibular Joint Disorder and improving your daily comfort.
Conclusion: Taking Control of Your Jaw Health
Temporomandibular Joint Disorder (TMD) is a multifaceted condition that can significantly impact your daily life, bringing jaw pain, headaches, and functional limitations. We’ve explored its long history, from ancient observations to modern scientific understanding, recognizing that it’s rarely caused by a single factor. Today, a combination of stress, injury, arthritis, and lifestyle habits can contribute to this common disorder. While controversies persist in diagnosis and treatment, particularly regarding the role of your bite and the choice between conservative and invasive therapies, the emphasis remains on evidence-based, reversible solutions.
Thankfully, a range of accepted treatments can provide relief, starting with simple self-care at home and progressing to non-surgical interventions like mouthguards, physical therapy, and medications. For persistent or severe cases, minimally invasive procedures or, as a last resort, surgery, offer further options. Looking forward, advances in 3D imaging, AI, regenerative medicine, and targeted drug therapies promise even more precise diagnostics and effective treatments. Taking charge of your jaw health means listening to your body and seeking professional help when needed. If you’re struggling with ongoing jaw discomfort or pain, consulting a healthcare professional is your crucial next step toward understanding and managing Temporandibular Joint Disorder.
FAQs About Temporomandibular Joint Disorder
Q1: What exactly is the difference between “TMJ” and “TMD”?
A1: “TMJ” refers to the temporomandibular joint itself, which connects your jaw to your skull. “TMD” (Temporomandibular Joint Disorder) is the umbrella term for conditions causing pain and dysfunction in these joints and surrounding muscles.
Q2: Can stress really cause my jaw to hurt?
A2: Yes, stress and anxiety are significant contributors to Temporomandibular Joint Disorder. They can lead to habits like jaw clenching or teeth grinding (bruxism), which put excessive strain on your jaw joints and muscles.
Q3: Are clicking or popping sounds in my jaw always a sign of Temporomandibular Joint Disorder?
A3: Not necessarily. While clicking or popping sounds can be a symptom of Temporomandibular Joint Disorder, they are common and often normal if they occur without pain or limited jaw movement. If these sounds are accompanied by discomfort or difficulty moving your jaw, you should seek professional advice.
Q4: What are the most effective home remedies for TMD pain?
A4: Simple self-care can be very effective. This includes eating soft foods, applying warm or cold packs to your jaw, avoiding habits like gum chewing, and practicing relaxation techniques to reduce jaw clenching.
Q5: Will I need surgery for my Temporomandibular Joint Disorder?
A5: Most people with Temporomandibular Joint Disorder find relief with conservative, non-surgical treatments. Surgery is typically reserved as a last resort for severe cases where other treatments have failed or for significant structural damage to the joint. Always get a second opinion before considering surgery.
Q6: What kind of doctor should I see for jaw pain?
A6: You can start by talking to your dentist or primary care physician. They can often diagnose Temporomandibular Joint Disorder and may refer you to a TMJ specialist, oral surgeon, or physical therapist for further evaluation and treatment.
Q7: Can Temporomandibular Joint Disorder cause headaches and ear pain?
A7: Absolutely. The jaw joints are close to your ears and connected to many facial and head muscles. Dysfunction in these areas can radiate pain, leading to frequent headaches (including migraines) and earaches that are not caused by infection.












Post Comment