When Your Body Whispers What Your Mind Can’t Say: Decoding Depression’s Physical Pain
Table of Contents

When Your Body Whispers What Your Mind Can’t Say: Decoding Depression’s Physical Pain
I’m here to talk about something crucial that many of us misunderstand: depression. We often think of it as purely an emotional struggle, something “in your head.” But what if I told you it’s a full-body experience? Sometimes, the first way depression shows up is as real, undeniable physical pain. This isn’t just discomfort you’re imagining; it’s a genuine, profound connection between your brain and your body that can dramatically impact your daily life, making simple tasks feel impossible. Understanding this link is the first step toward finding comprehensive relief.
The Enduring Story of the Aching Mind: A Historical View
For centuries, people have tried to understand the mysterious link between our minds and our bodies. How could a feeling cause a backache? Let’s trace this understanding through history.
Ancient Insights and the Humoral Theory
Way back in ancient Mesopotamia, folks often believed that bad spirits caused conditions similar to depression and their physical woes. Priests, not physicians, were the ones to address these spiritual ailments. However, a significant shift happened in ancient Greece. Hippocrates, often called the father of medicine, offered a more scientific explanation for “melancholia”—what they called depression. He suggested it came from an imbalance of the four bodily humors, specifically an excess of “black bile.” Hippocrates noted both mental and physical symptoms, including “fears and despondencies,” along with poor appetite and restless nights. Galen, a Roman physician, further expanded on this, observing that a poor mental state could make people physically ill, noting individuals becoming sick due to anger, confusion, distress, and fright. This ancient wisdom, therefore, recognized that our emotional state could indeed manifest as physical illness.
The Great Divide: Mind and Body Separate
Fast forward to the Renaissance, and philosopher René Descartes introduced a powerful idea that deeply influenced Western medicine: the mind and body were totally separate entities. He proposed they interacted only at a single point, the pineal gland. This concept, often called the “Cartesian mind/body split,” made it tough for doctors for centuries to see how your feelings could actually make your back hurt or cause other bodily aches. The focus shifted, often treating the body and mind as independent systems. For a long time, if you went to the doctor with a physical ache, the idea that it might be connected to your mental state was often overlooked. This dualistic view led to a fragmented approach to healthcare, where physical and mental health were addressed in isolation.
Coming Together: A Holistic View
Thankfully, in the 20th century, we started realizing that the mind and body are constantly chatting, influencing each other in profound ways. Modern science now sees depression as a complex mix of biology, thoughts, and life experiences, all intricately connected to physical symptoms. We understand that our brain, nervous system, and immune system are in continuous communication, and disruptions in one area can ripple through others. This integrated understanding is crucial, recognizing that genuine well-being requires acknowledging the whole person—mental and physical. The outdated idea of a strict separation between mind and body is being replaced by a more holistic view that recognizes their inherent and deep connection, paving the way for more effective treatments.
The “Ouch” List: Where Depression Can Hit Your Body
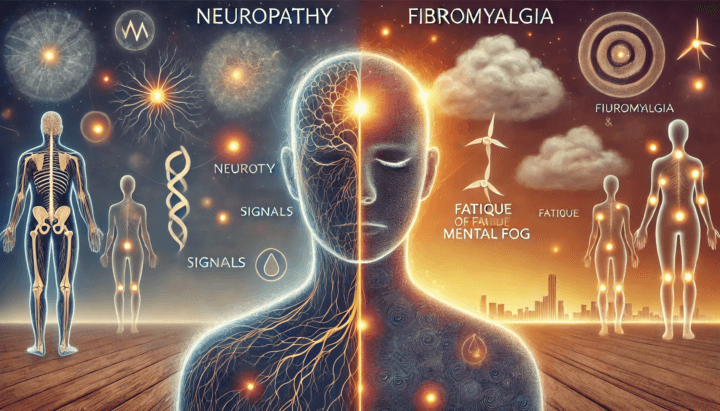
When depression takes hold, it’s not just your thoughts and emotions that are affected; your body often feels it loud and clear. Your brain uses special messengers, called neurotransmitters like serotonin and norepinephrine, for both mood and pain. When depression messes with these, your body can become more sensitive to pain, turning a small ache into a big deal.
Common Painful Manifestations
Depression can present with a variety of physical pains, often mimicking other medical conditions, which can make it hard to diagnose. Here are some common ways depression can cause physical discomfort:
- Headaches that Won’t Quit: Many people with depression experience headaches, ranging from nagging tension headaches to pounding migraines. These can be particularly bothersome and are often worse with stress. Up to 40% of people with migraines also suffer from depression, highlighting a significant link.
- That Persistent Backache: Back pain is a frequently reported symptom of depression. This isn’t imaginary pain; it’s a real physical manifestation, potentially influenced by inflammation and the impact of depression on muscle tension and posture. It’s often a sneaky symptom, and a real pain in the… well, you know.
- Generalized Aches: You might find your muscles and joints protesting for seemingly no reason. This can include widespread muscle aches and joint pain, often described as a dull, aching sensation that can worsen during periods of stress or heightened anxiety. Depression can lower your pain tolerance, making normal aches feel more intense.
- Gut Reactions: The gut-brain highway is incredibly busy! Emotional distress directly influences digestive health. Depression can lead to symptoms like nausea, indigestion, diarrhea, constipation, stomach cramps, and even irritable bowel syndrome (IBS). Changes in gut bacteria due to stress can also contribute to these digestive issues.
- Chest Tightness: While chest pain should always be evaluated by a doctor to rule out serious heart or lung conditions, sometimes it’s your feelings making your chest hurt. It can be a symptom of anxiety often co-occurring with depression, mimicking more severe conditions.
- More Than Just Pain: Beyond specific aches, depression also brings a host of other physical symptoms that can profoundly impact daily life:
- Extreme Exhaustion and Fatigue: This isn’t just tiredness that sleep can fix. It’s a pervasive lack of energy, making even simple activities like getting out of bed seem impossible. Over 90% of individuals with major depressive disorder experience severe fatigue.
- Sleep Disturbances: Depression frequently causes troubled sleep, whether it’s difficulty falling or staying asleep (insomnia), waking up too early, or sleeping much more than normal (hypersomnia). Poor sleep quality exacerbates both pain and depressive symptoms.
- Weird Appetite Changes: You might notice a significant loss of appetite and weight loss, or conversely, increased cravings for certain foods (often carbohydrates) and weight gain.
- Dizziness or Lightheadedness: Some individuals with depression may experience these sensations without a clear physical cause.
- Decreased Interest in Sex (Low Libido): A reduced sex drive is another common physical symptom linked to depression.
- Psychomotor Activity Changes: This can manifest as noticeable slowing of physical movements and speech, making it challenging to function.
These physical symptoms can be challenging to diagnose as being linked to depression because they often mimic other medical conditions, leading many to seek treatment for physical ailments without realizing the underlying emotional cause. Addressing both emotional and physical symptoms is crucial for effective treatment.
Why the Confusion? Debates and Unanswered Questions
The intricate link between depression and physical pain presents many complexities, leading to ongoing discussions and questions within the medical and scientific communities.
The Chicken or Egg Dilemma: Causality Challenges
One of the most persistent questions is: Does depression cause pain, or does chronic pain make you depressed? It’s a tricky loop, and scientists are still figuring out the exact sequence. What they agree on is that it’s a two-way street. Chronic pain is a significant stressor that can wear a person down, affecting sleep, work, and social life, thus increasing the risk of depression. Conversely, depression can lower your pain threshold, making you more sensitive to physical discomfort. Some research even suggests that depressive feelings and loneliness can show up years before pain becomes a real problem, indicating that early mental health interventions might prevent later chronic pain. This bidirectional relationship makes untangling the primary cause in any individual case quite difficult.
The Doctor’s Dilemma and Stigma
When you visit a doctor and only talk about your knee pain, headaches, or stomach issues, it’s easy for depression to fly under the radar. Physical symptoms often take precedence in clinical settings, and healthcare providers might focus solely on the bodily complaint, missing the underlying mood disorder. There’s still a persistent stigma that makes it hard for people to connect their physical aches to their emotional state. Many patients fear being dismissed or told their pain is “all in their head,” leading them to hesitate discussing mental health symptoms. This reluctance means depression can go undiagnosed and untreated, which, in turn, can worsen existing pain and other physical symptoms, creating a vicious cycle of suffering.
Finding the Right Fix: Integrated Treatment Challenges
Because pain and depression have often been studied and treated separately, finding integrated treatments has been a puzzle. Traditional clinical trials frequently excluded individuals with both conditions, creating a gap in research. We’re still trying to understand the precise role of inflammation: does depression cause inflammation, or does chronic inflammation predispose you to depression? Both seem true to some extent, with chronic stress and depression linked to elevated inflammatory markers. This complexity means that a single, one-size-fits-all solution is unlikely.
Opioid Worries: A Double-Edged Sword
There’s a significant discussion around using powerful painkillers, like opioids, for chronic pain when depression is in the picture. While they can offer temporary relief, long-term opioid use can sometimes make depression worse or lead to addiction. Research shows a documented link between depression and opioid misuse, with depression intensifying physical pain and heightening cravings. This creates a critical dilemma for healthcare providers trying to manage both conditions without introducing new risks or exacerbating existing ones. It underscores the need for comprehensive, non-addictive pain and mood management strategies.
Paving New Paths to Relief: Innovative Treatments for Mind and Body
The good news is that we’re getting smarter about tackling both pain and depression together, recognizing their shared pathways. Innovative treatments are focusing on integrated care to provide more effective and lasting relief.
Collaborative Care and Smart Medications
The medical community is increasingly adopting integrated care, where doctors, therapists, and other specialists work as a team to treat the whole you. This collaborative approach ensures that both your physical and mental health needs are addressed simultaneously.
When it comes to smart meds, certain antidepressants are proving to be multitaskers. Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), like duloxetine and venlafaxine, are often recommended as first-line pharmacological treatments. They hit those shared brain pathways, improving both mood and pain by balancing neurotransmitters that influence both conditions. Tricyclic antidepressants (TCAs) such as amitriptyline and nortriptyline also show efficacy in various neuropathic pain conditions, even at low doses for pain management. While Selective Serotonin Reuptake Inhibitors (SSRIs) like fluoxetine primarily target mood, SNRIs and TCAs offer the added benefit of pain relief.
Mind Power: Therapeutic Approaches
Beyond medication, powerful psychological therapies are game-changers in managing the mind-body connection:
- Cognitive Behavioral Therapy (CBT): This therapy teaches you to understand how your thoughts, feelings, and behaviors are interconnected. For pain and depression, CBT helps you identify and reshape negative thought patterns that intensify pain perception and contribute to low mood. It promotes healthy coping mechanisms, leading to reduced suffering and improved quality of life. My patient, Sarah, used to dread waking up because her chronic back pain felt insurmountable. Through CBT, she learned to challenge catastrophic thoughts like “This pain will ruin my entire day” and instead focus on small, manageable steps, which significantly reduced her overall distress.
- Acceptance and Commitment Therapy (ACT): ACT encourages you to accept discomfort and challenging thoughts rather than fighting them. It helps clarify your personal values and commit to actions aligned with those values, even when pain is present. This approach helps individuals acknowledge discomfort as part of behavioral change, showing promise in reducing pain, improving depression, and potentially decreasing reliance on pain medication.
- Mindfulness-Based Stress Reduction (MBSR): MBSR cultivates present-moment awareness and acceptance through practices like meditation and gentle yoga. It helps you observe thoughts and feelings without judgment, significantly reducing pain intensity and symptoms of depression, while also improving mood and sleep. “I used to feel trapped by my anxiety and the constant pressure in my chest,” shared David, a client of mine. “Learning mindfulness helped me create space between my feelings and my reaction, allowing me to breathe and respond more calmly.”
Beyond the Couch: Emerging and Complementary Therapies
The landscape of treatment is expanding with exciting new options:
- Ketamine Therapy: For really tough cases of depression and chronic neuropathic pain, low-dose ketamine therapy is an exciting, emerging option. It works by blocking certain brain receptors, leading to rapid antidepressant effects and sustained changes in mood and consciousness, often when integrated with psychotherapy.
- Virtual Reality (VR): Yes, really! VR can distract your brain from pain and anxiety. Immersing patients in calming virtual environments has been shown to reduce pain and anxiety, and can even improve physical function by shifting focus away from discomfort.
- Brain Zaps (TMS): Transcranial Magnetic Stimulation (TMS) is a non-invasive neuromodulation technique that uses electromagnetic pulses to stimulate underactive brain areas involved in mood regulation. It can help reset brain areas linked to depression, especially for those who haven’t responded to medication.
- AI to the Rescue: Artificial intelligence is revolutionizing pain management by analyzing vast patient data to help craft personalized treatment plans, predict outcomes, and optimize interventions, promising more targeted and effective strategies.
- Move Your Body: Physical activity is a powerful tool. Exercise, yoga, tai chi, and even acupuncture and massage are getting deserved recognition for their ability to soothe both body and mind. Regular movement stimulates endorphin release, reduces stress hormones, improves sleep, and boosts self-esteem, all of which benefit mental health and pain management. For Maria, who struggled with generalized body aches, a consistent yoga practice not only eased her physical discomfort but also brought a sense of calm she hadn’t experienced in years.
- Acupuncture: This traditional Chinese medicine technique, involving the insertion of thin needles into specific body points, aims to balance energy flow and has been suggested to reduce symptoms of pain, insomnia, and depression.
These diverse approaches underscore the move towards comprehensive, personalized treatment strategies that respect the complex interplay between our mental and physical well-being.
The Horizon: What’s Next for the Mind-Body Connection
The future of understanding and treating the link between depression and physical pain is bright, with scientific research continually unveiling deeper connections and more targeted solutions. We are moving towards a healthcare model that truly treats the entire person.
Unlocking the Body’s Clues: Biomarkers and Early Intervention
Scientists are tirelessly hunting for “biomarkers” – tiny clues in your body like inflammatory proteins or specific genes – that could help diagnose issues earlier and create super-targeted treatments. Imagine this: detecting changes in your body chemistry that signal a predisposition to depression years before psychological symptoms or chronic pain even strike! Research has shown that worsening depressive symptoms and loneliness can precede the onset of moderate to severe pain by up to eight years in middle-aged and older adults. This highlights a crucial focus for future research: catching depressive symptoms early could actually prevent chronic pain from developing. Early mental health and social support interventions could make a profound difference, potentially reducing or delaying the later onset of physical aches and pains. This preventive approach is a huge focus for future research and early interventions.
Tailoring Treatment: Personalized Medicine and Holistic Care
We’re moving towards truly personalized medicine, understanding how your unique genetics, neurobiology, and even your life experiences affect your pain and mood. AI, for instance, is helping analyze vast patient data to develop customized treatment plans and predict outcomes. This means treatments could soon be tailored precisely to your individual profile, optimizing effectiveness and minimizing side effects.
The ultimate goal? Holistic care models that treat the entire person, making sure everyone has access to the support they need, not just for their mind, but for their whole self. This includes multidisciplinary teams working together, incorporating insights from psychoneuroimmunology (the study of the interaction between psychological processes and the nervous and immune systems) and epigenetics to develop targeted therapies. These models aim to overcome the current fragmentation of care, leading to improved outcomes for those experiencing both depression and chronic pain. Accessibility is key, especially for vulnerable populations with fewer socioeconomic resources who often face greater challenges in accessing mental health and pain management support.
The journey to better health involves recognizing that our bodies and minds are inseparable. As we continue to unravel these intricate connections, we gain powerful new ways to find relief and live fuller, more comfortable lives. If you or someone you know is experiencing persistent physical pain alongside symptoms of depression, know that integrated support is available.











Post Comment