What Everyone Needs to Know About Temporomandibular Joint Disorder (TMD)
Table of Contents
Your Jaw, Unlocked: What Everyone Needs to Know About Temporomandibular Joint Disorder (TMD)
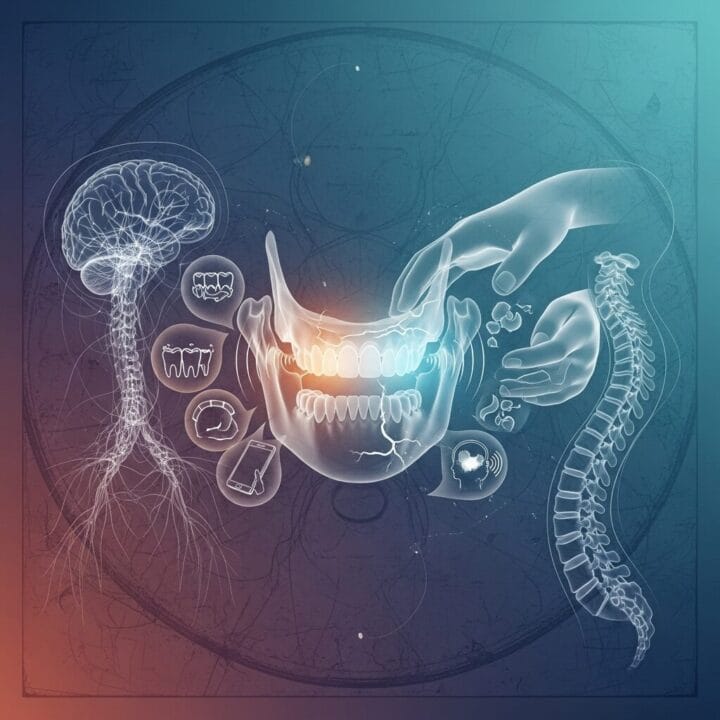
I’ve met many people grappling with jaw pain, those clicking sounds, or headaches that seem to come from nowhere. You might wonder, “What exactly is wrong with my jaw?” Or perhaps, “Why does my jaw lock when I try to eat?” These are questions about temporomandibular joint disorder, known as TMD. This condition affects millions, creating significant discomfort and often confusion. I want to break down TMD simply, explain what it means for you, and clarify how medical professionals approach it today, moving past outdated ideas and into what truly helps people with this persistent jaw pain.
What’s That Clicking Sound? Getting to Know Your TMJ and TMD
My patients frequently ask about the joint itself. “Is it my TMJ acting up?” they inquire. It helps to clarify the terminology.
The Joint and the Disorder: Understanding Temporomandibular Joint Disorder
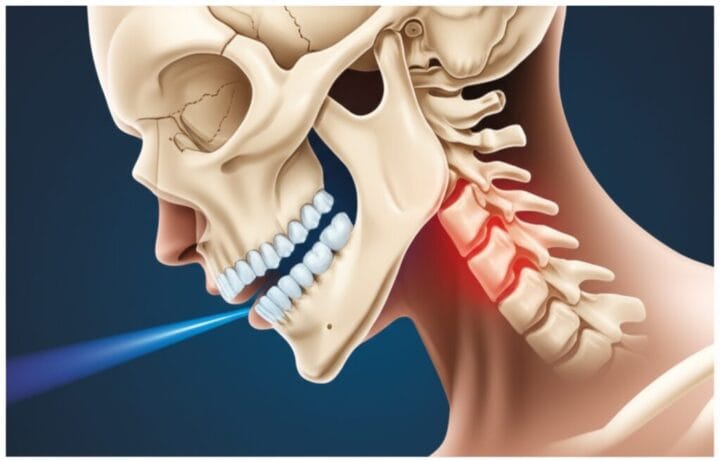
The TMJ refers to the temporomandibular joint itself. I think of it as a sliding hinge that connects your lower jaw, the mandible, to your skull. You have two of them, one on each side, right in front of each ear. These joints allow my jaw to move up and down, side to side, and forward and back, making it possible for me to talk, chew, and yawn. Now, TMD, or temporomandibular joint disorder, is a collective term for a group of over 30 conditions that cause pain and dysfunction in these joints and the muscles that control jaw movement. It’s not a single problem, rather a collection of issues that can affect your jaw’s function and well-being.
Who’s Affected by Jaw Pain?
This condition is far from rare. Consider this: up to 12 million Americans experience TMD symptoms. It frequently appears between the ages of 20 and 40. For some reason, women are twice as likely to have it than men, which is something research continues to study. My experience tells me that stress often plays a starring role in bringing these symptoms to the surface. For many people, understanding they are not alone in their discomfort brings a measure of relief.
The Laundry List of Annoyances for Your Jaw
The symptoms of TMD are diverse, sometimes mimicking other conditions, which complicates accurate TMD diagnosis. Patients describe jaw pain that ranges from a dull ache to sharp, intense discomfort. Many experience facial pain, neck aches, and shoulder stiffness that radiates from the jaw. Headaches, often severe, can even be mistaken for migraines. I hear reports of unusual clicking, popping, or grinding sounds when opening or closing the mouth. These sounds are only clinically important if accompanied by pain or limited movement.
Other common issues include jaw stiffness, lockjaw—where your jaw gets stuck in either an open or closed position—and difficulty chewing food. Earaches, a sense of fullness in the ear, or ringing in the ears (tinnitus) are also frequently reported, even without an ear infection. Occasionally, I’ve heard patients mention dizziness, a truly disorienting experience. “My jaw just feels wrong,” a client told me recently. “It’s like it’s fighting itself every time I try to talk or eat.” These myriad symptoms underscore the need for a comprehensive view of temporomandibular pain.
Why Me?! The Usual Suspects Causing Temporomandibular Pain
It’s seldom one isolated incident, this jaw discomfort. Often, a combination of factors conspires to bring about TMD. One common culprit is teeth grinding or clenching, medically known as bruxism. Many do this unconsciously, especially at night, putting immense strain on the jaw joints and muscles. A direct jaw injury or trauma to the head or neck can certainly initiate problems. Arthritis, much like in other joints, can affect the TMJ.
Stress and anxiety are immense contributors. When I am stressed, I notice myself clenching my jaw. This tension, when sustained, impacts the muscles surrounding the jaw joint. Poor posture, particularly the “phone neck” position many adopt while looking at screens, can strain the neck and jaw muscles, exacerbating problems. Sometimes, a small disc inside the joint slips out of place, causing clicking and pain. My advice to anyone experiencing these issues is to consider the broader context of their daily habits and stressors. “I never thought my work deadlines were causing my jaw to hurt until I realized I was grinding my teeth all night,” one individual shared with me, highlighting the connection.
From “Costen’s Syndrome” to Modern Mysteries: A Brief History of Jaw Issues
Old School Jaw Woes
It feels like jaw pain is a modern affliction, but humans have faced jaw issues for millennia. Ancient texts from Egypt and Greece mention remedies for jaw discomfort. Early descriptions of mechanical jaw problems, like disc issues, surfaced in the late 1800s. These early observations were rudimentary, yet they show that the enigma of jaw pain has long puzzled humanity. I often ponder how frustrating it must have been to live with such pain without the diagnostic tools we possess today.
The Dental Connection (and Misdirection) in TMD Diagnosis
A critical historical moment arrived in the 1930s with Dr. James Costen. An ENT physician, he linked a cluster of seemingly unrelated symptoms—headaches, facial pain, ear ringing, and vertigo—to problems with the temporomandibular joint. He theorized these issues, soon dubbed “Costen’s Syndrome,” were caused by missing back teeth. This put dentists in the driver’s seat for quite some time, leading to various dental-focused treatments. Many of these treatments, designed to “fix the bite,” were experimental and often unhelpful, sometimes even causing irreversible alterations. This era, in my opinion, highlights the danger of oversimplified theories for complex conditions.
The “It’s All In Your Head” Era
Imagine experiencing chronic, debilitating jaw pain, only to be told it’s “all in your head.” For a significant period, if doctors couldn’t find a clear physical cause for jaw pain, patients were often dismissed, their suffering attributed to psychological factors. This deeply frustrating and disempowering approach undoubtedly delayed genuine research and effective interventions for many. I find this aspect of medical history particularly disheartening, a reminder of the importance of listening to patients.
A Broader View Emerges for Jaw Pain
Fortunately, the tide began to turn by the 1980s. We started recognizing that TMD isn’t just a simple mechanical issue or purely about teeth. It’s a complex interplay of physical, psychological, and even social factors. This shift led to what we call the “biopsychosocial model.” This means clinicians consider biological elements (like joint damage or muscle tension), psychological aspects (such as stress, anxiety, or depression), and social influences (like daily habits or work environments). This holistic approach, I believe, has revolutionized how we understand and manage temporomandibular pain, offering a more complete picture for those seeking help.
Your Jaw Today: Current Medical Approaches to TMD Treatment
First, Let’s Talk: TMD Diagnosis
When someone comes to me with potential TMD, my initial step is always a conversation. I ask about the symptoms: where is the pain? When does it occur? What makes it better or worse? Does the jaw click or lock? Your story is critical; it paints the initial picture. Following this, I conduct a physical exam, checking the jaw’s movement, feeling for tenderness in the muscles and joint, and listening for any sounds.
Sometimes, for more intricate cases, imaging like MRIs or CT scans provides a clearer view of the joint’s internal structures. However, these are not always necessary. The Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) now provides a standardized way for professionals to diagnose, categorizing painful conditions like muscle pain or headache related to TMD, and joint issues such as disc displacement. This structured approach helps ensure a thorough evaluation.
Keeping it Simple (and Reversible!): TMD Management Strategies
The guiding principle in modern TMD care is “conservative first, and reversible.” I advocate for starting with the simplest, least invasive methods. Many cases of TMD improve significantly, or even resolve completely, with these initial steps. Think about incorporating soft foods into your diet to give your jaw a rest. Applying heat or ice packs to the jaw can soothe discomfort and reduce inflammation. Gentle jaw exercises, often guided by a physical therapist, can restore function and ease muscle tension. Crucially, managing stress is a powerful tool. Techniques like deep breathing, mindfulness, or regular exercise directly impact jaw clenching habits. One patient found immense relief simply by consciously practicing keeping their teeth apart throughout the day. It’s about empowering individuals with practical, everyday solutions for their temporomandibular pain.
Splints and Nightguards for Jaw Clenching
Many people use oral appliances like splints or nightguards. These custom-fitted devices fit over the teeth, often worn at night, and serve a few purposes. Primarily, they protect the teeth from grinding and clenching, habits that put significant strain on the TMJ. They might also help relax jaw muscles and, in some instances, subtly reposition the jaw to relieve pressure.
However, I emphasize a critical point: these appliances should never permanently alter your bite. While useful for symptom management, the scientific community continues to debate their overall effectiveness for long-term pain relief. Some research suggests their benefit might stem partly from a placebo effect or simply by increasing awareness of clenching habits. If an appliance causes new pain or changes your bite, it is important to consult a dentist immediately.
Beyond the Jaw: Comprehensive TMD Care
Modern care extends beyond just the jaw itself. I see it as a holistic undertaking. Physical therapy is often invaluable, providing exercises to improve jaw mobility and reduce muscle spasms. Therapists might use techniques like massage or dry needling. Stress-busting strategies, such as Cognitive Behavioral Therapy (CBT), help individuals identify and change behaviors that worsen pain, offering significant long-term advantages. Medications, including over-the-counter pain relievers or prescription muscle relaxers, can offer temporary relief. In some cases, injections like corticosteroids or Botox into specific jaw muscles can help reduce tension and pain. A truly comprehensive approach addresses not just the physical symptoms but also the emotional and behavioral factors contributing to the temporomandibular disorder.
“No Permanent Changes, Please!”: Avoiding Irreversible Jaw Treatments
This point cannot be overstated. A major shift in current medical thinking strongly advises against treatments that permanently alter your jaw or teeth. This includes procedures like grinding down tooth enamel for “bite adjustments” or unnecessary orthodontic treatments solely for TMD. The science simply does not support these irreversible interventions as effective long-term solutions for TMD, and they can, in fact, cause more harm than good, creating new, complex problems. “I regret getting my teeth ground down,” a patient once confessed, “it made my jaw pain worse, and there’s no going back.” I strongly encourage anyone considering such treatments to seek multiple opinions and prioritize conservative options first.
Surgery for TMD? Only If You Really Have To
When dealing with TMD, I view surgery as a definitive last resort. It’s considered only for severe structural problems within the joint that have failed to respond to all other conservative treatments. Even then, caution is my watchword. Procedures like arthrocentesis (flushing the joint) or arthroscopy (minimally invasive joint exploration) are less invasive but still carry risks. Open-joint surgery, for issues like joint erosion or a frozen joint, is a major procedure with a longer recovery time and potential for complications. It’s imperative to have clear, specific indications before considering such a step.
Jaw-Dropping Debates: The Big Fights in TMD Science
What Really Causes Temporomandibular Disorder?
The exact causes of TMD remain a hot topic, sparking vigorous debate among experts. While we agree it is multifactorial, the specific contributions of individual elements are often questioned. The role of one’s bite, or occlusion, is particularly controversial. For years, some believed that a “bad bite” was the primary cause, leading to extensive dental procedures. Today, most experts largely refute this, stating that occlusal issues are rarely the main culprit. Many individuals with misaligned bites never develop TMD. Even the connection between teeth grinding (bruxism) and TMD pain is debated; self-reported grinding might show a link, but more objective measures sometimes reveal a weaker association. The intricate interplay of factors makes pinning down a single cause incredibly challenging.
Hard to Pin Down: TMD Diagnostic Challenges
TMD is notoriously tricky to diagnose. Its symptoms can mimic many other conditions, creating a diagnostic labyrinth. Is it a toothache? Sinus problem? Migraine? Ear infection? The overlapping symptoms mean that a precise TMD diagnosis demands careful differentiation. Furthermore, it’s not uncommon for patients to present with multiple issues concurrently, making a clear-cut diagnosis even more elusive. The journey to effective treatment often begins with ruling out various possibilities, a process that can feel like solving a complex puzzle for both the patient and the clinician.
Are We Over-Treating TMD Symptoms?
This is a pertinent question I often contemplate. Given that many TMD cases are temporary and resolve spontaneously, or respond well to simple self-care, are we sometimes too quick to intervene with complex or costly treatments? The high rate of spontaneous remission makes it challenging to definitively say whether a particular treatment “worked” or if the body simply healed itself. This ambiguity fuels debates about when to intervene, and with what specific modality, especially when considering more advanced or irreversible options. It brings me back to my core belief: conservative approaches first.
The Gender Gap in Jaw Pain
The fact that TMD affects women more frequently, particularly those between 20 and 40, raises important questions. Historically, this gender disparity unfortunately led to some opinions dismissing women’s pain or attributing it to psychological factors, an approach I find unacceptable. This bias has undoubtedly hampered research efforts, slowing our understanding of why women are more susceptible. Today, we recognize this gap and strive for more inclusive research to identify potential biological and hormonal contributions to temporomandibular pain. It is an area that requires more focused investigation to ensure equitable care.
Unproven “Cures” for TMD
In the landscape of TMD care, some “cures” lack scientific backing. I urge extreme caution against fancy diagnostic gadgets or treatments that promise quick fixes by permanently altering your bite or jaw structure. These interventions, often expensive, frequently lack robust scientific evidence. They can even cause more harm than good, leading to irreversible damage or persistent pain. Relying on scientifically validated, conservative approaches is always the most responsible path when dealing with temporomandibular disorder.
Peering into the Jaw Crystal Ball: What’s Next for TMD Research?
Smarter TMD Diagnostics
The future of TMD diagnosis is exciting. Imagine a world where 3D imaging, like advanced CBCT, provides incredibly detailed views of your jaw joint, precisely identifying even subtle abnormalities. Think about AI software analyzing your symptoms, medical history, and scans in real-time, offering instant, personalized insights. These computer-aided diagnostics could revolutionize how quickly and accurately we pinpoint the specific issue behind your jaw pain. Researchers are even exploring non-invasive methods, like analyzing salivary endocannabinoid profiles, to screen for TMD. This means less guesswork and more precise, targeted care.
Gentler Fixes for Jaw Problems
I anticipate a strong move towards minimally invasive therapies. Procedures like Botox injections, already gaining traction, will likely become more refined to relax specific jaw muscles, offering targeted relief from tension. Arthrocentesis, flushing out the joint with a sterile solution, is another gentle technique gaining recognition for its ability to reduce inflammation and debris with minimal risk. We’re seeing more research into laser therapy and ultrasound, non-invasive methods that use light or sound waves to reduce pain, inflammation, and promote tissue regeneration in the joint. These advancements aim to offer effective relief with less downtime and discomfort for people suffering from temporomandibular pain.
Rebuilding Your Jaw: Regenerative Therapies
The frontier of regenerative medicine offers truly groundbreaking possibilities for TMD. Imagine treatments that don’t just manage symptoms but actively repair damaged jaw tissues. Platelet-Rich Plasma (PRP) and Platelet-Rich Fibrin (PRF) therapies are already being explored. These treatments use concentrated growth factors from your own blood to kickstart healing and reduce inflammation in the joint. The potential for stem cell therapy to regenerate damaged cartilage or even grow new jaw discs is a truly captivating prospect. This field aims to move beyond temporary fixes, offering solutions that could fundamentally restore the health of the temporomandibular joint.
Tech-Enhanced Self-Care for TMD Patients
Personalized self-care, amplified by technology, is on the horizon. Picture a future where you have a 3D-printed splint, perfectly molded to your unique anatomy, perhaps even embedded with sensors to track your jaw movements and clenching patterns throughout the night. Smartphone apps, powered by AI, could become your personal TMD coach, offering tailored stress management techniques, gentle exercises, and real-time feedback based on your individual symptoms and habits. This blend of cutting-edge technology and accessible self-management tools promises a more proactive and effective way for individuals to manage their temporomandibular disorder daily.
The NIH Is On It!
It’s encouraging to see significant efforts from major research institutions. The National Institutes of Health (NIH), for instance, is actively funding initiatives like the “TMD Collaborative for Improving Patient-Centered Translational Research (TMD IMPACT).” These initiatives aim to conduct new clinical trials, establish comprehensive patient registries, and develop clear, evidence-based clinical practice guidelines. The goal is to better predict who responds best to which treatment, identify the genetic and physiological roots of TMD pain, and ultimately deliver more effective, individualized care for those with temporomandibular joint disorder. This large-scale, coordinated research is essential for moving the field forward.
More Than Just a Jaw: Personalized TMD Care
The overarching direction for TMD care is a deeply personalized, multidisciplinary approach. This means moving beyond a one-size-fits-all model, recognizing that each person’s experience with temporomandibular disorder is unique. It requires a comprehensive view of your entire health picture—your physical body, your mental well-being, and your lifestyle. By integrating insights from advanced diagnostics, minimally invasive treatments, regenerative therapies, and tech-enhanced self-care, all guided by ongoing research, the future promises truly individualized care that maximizes relief and minimizes discomfort.
TMD is a complex condition, yet remarkable progress in understanding and managing it continues. I encourage you to seek out healthcare professionals who embrace a modern, conservative, and multidisciplinary approach. Don’t settle for irreversible treatments unless absolutely necessary. Your jaw’s comfort and long-term health depend on informed choices and effective temporomandibular joint disorder solutions.
For more information, visit: National Institute of Dental and Craniofacial Research (NIDCR)












Post Comment