Meniere’s Disease: Understanding the Inner Ear’s Unpredictable Storm
Table of Contents
Meniere’s Disease: Understanding the Inner Ear’s Unpredictable Storm
I can tell you, dealing with Meniere’s disease means living with a world that spins on its own axis, often without any notice. It means confronting a persistent ringing in your ears, hearing that drifts in and out like a radio signal, and a sensation in your ear that feels like cotton, thick and insistent. This condition, a chronic inner ear disorder, throws balance and hearing into disarray, a relentless adversary for anyone experiencing its grip. These Meniere’s episodes appear with startling suddenness, stretching from twenty minutes to a full day, each one a testament to the brutal, sometimes disorienting, power it holds. They can even manifest as “drop attacks,” moments where your body simply gives way, collapsing without warning. Typically, this affliction begins its insidious work in one ear, usually striking individuals between 40 and 60 years of age, yet for a considerable portion of those affected—about 15-30%—it eventually takes hold in both ears, extending its reach further into their lives.
A Glimpse into the Past: Meniere’s Disease Through Time
The very notion of Meniere’s disease, as we understand it, has a history extending back centuries, although the precise classification emerged relatively recently. People, it seems, grappled with sudden, disorienting spells of dizziness since ancient Roman eras; one might even consider historical accounts of figures like Julius Caesar’s reported “giddiness” and hearing difficulties as ancestral whispers of this same affliction. However, it was Prosper Menière, a French physician of sharp intellect, who, in 1861, pieced together these disparate observations. He dared to propose a revolutionary concept: that these severe vertigo episodes, previously believed to originate from the brain’s mysterious workings, actually stemmed from the inner ear. A truly radical idea, the medical establishment took nearly seven decades to fully embrace its profound implications.
My own grandmother, who for years dismissed her intermittent bouts of spinning as “just getting old,” found solace in learning of Menière’s early assertions. “Someone finally put words to it,” she told me, a faint smile touching her lips, “that it wasn’t all in my head, a trick of the mind.”
Then, in 1938, a crucial breakthrough offered a physical manifestation for Menière’s clinical theories. Hallpike and Yamakawa, working independently, identified a peculiar phenomenon: endolymphatic hydrops, an abnormal accumulation of fluid within the inner ear. This discovery unveiled what was structurally amiss. Fast forward to 2007, and advanced MRI technology transformed this understanding, allowing us to visualize this very fluid buildup in living patients, bridging the gap from post-mortem observation to real-time clinical insight. This progression in our ability to see and understand the physical reality of Meniere’s disease has been monumental, changing the landscape of diagnosis and research.
The Inner Ear’s Puzzle: What Causes Meniere’s Disease?
The most prominent factor driving Meniere’s disease symptoms appears to be the aforementioned endolymphatic hydrops—a significant surplus of fluid within the inner ear’s intricate labyrinth. This excess, a disruption of the delicate balance between endolymph and perilymph, profoundly skews the sensitive signals that govern our balance and hearing. Imagine a finely tuned instrument suddenly filled with too much water; its ability to produce clear sound or maintain equilibrium would be compromised. That’s essentially what happens with Meniere’s disease, creating a cacophony of symptoms.
Yet, the ultimate genesis of this fluid accumulation continues to puzzle medical minds. Doctors grapple with several compelling theories, each a potential thread in this complex biological tapestry:
- Vascular Constraints: Could restricted blood vessels, mirroring the vascular changes observed in certain migraines, be triggering a localized, miniature migraine event within the ear? This idea posits an ischemic origin, where reduced blood flow predisposes the inner ear to hydrodynamic changes.
- Biological Agents: Perhaps viral infections or even subtle autoimmune reactions, where the body’s defenses mistakenly attack inner ear tissues, contribute to the fluid imbalance. Allergy responses are also explored, suggesting an immune system link.
- Drainage Issues or Injury: Some hypothesize blockages obstruct the normal drainage of inner ear fluid, or perhaps head injuries precipitate the condition by disrupting the delicate hydraulic system.
- Genetic Factors: We observe Meniere’s disease running in families for about 7-10% of cases, hinting at a genetic predisposition. Certain gene mutations, such as GJD3, have been identified, pointing toward inherited susceptibility and potentially offering future avenues for targeted therapies.
The fluid buildup itself remains a central figure, its origin shrouded in ambiguity, making the Meniere’s disease landscape complex, full of scientific debate and differing perspectives among researchers. It is a condition where the “why” often precedes the “how,” and understanding these potential influences becomes crucial for future therapeutic design.
Detecting the Unseen: How Doctors Diagnose Meniere’s Disease
Diagnosing Meniere’s disease is not a straightforward affair, lacking a single definitive marker like a quick blood test. Instead, it resembles a meticulous detective process, a puzzle where many pieces must align. A “eureka!” moment is rare, replaced by careful evaluation and the exclusion of other conditions. My friend, Mark, described his diagnostic journey as “trying to find a ghost in a machine that’s always changing its parts.” That, I think, captures the essence.
Clinicians rely heavily on your personal account of symptoms and a precise pattern of events to arrive at a diagnosis of Meniere’s disease. Key elements include:
- Recurrent Vertigo Episodes: You must have experienced at least two spontaneous vertigo episodes, each lasting between 20 minutes and 12 hours. This sustained, debilitating spinning sensation is a cornerstone of the Meniere’s picture.
- Hearing Loss Evidence: Documented low-to-medium frequency sensorineural hearing loss in the affected ear, confirmed by audiometry, must be present on at least one occasion before, during, or after a vertigo episode. This fluctuating hearing is a distinguishing feature.
- Other Aural Symptoms: Accompanying symptoms like tinnitus (ringing, buzzing, or roaring in the ear) or a feeling of aural fullness (pressure or congestion in the ear) further complete the diagnostic criteria.
- Exclusion of Other Conditions: Critically, these symptoms must not be more accurately explained by another vestibular disorder. This “diagnosis of exclusion” can be frustrating, as many conditions, such as vestibular migraines, transient ischemic attacks (TIAs), or even certain types of brain tumors, can mimic Meniere’s disease symptoms, making differentiation an intricate task.
To aid in this investigative process, doctors employ various tools:
- Audiometry: These hearing tests measure your ability to hear different pitches and volumes, helping to identify the characteristic low-frequency hearing loss linked to Meniere’s disease.
- Balance Assessments: Tests like videonystagmography (VNG) or vestibular evoked myogenic potentials (VEMP) evaluate the function of your inner ear’s balance system, pinpointing potential dysfunction.
- Imaging Scans: MRI or CT scans of the brain are often conducted to rule out other, potentially serious, conditions that could present with similar symptoms, ensuring nothing else is masquerading as Meniere’s.
It is this rigorous, multi-faceted approach, balancing subjective patient reports with objective clinical findings, which allows for the confirmation of Meniere’s disease, guiding subsequent management strategies.
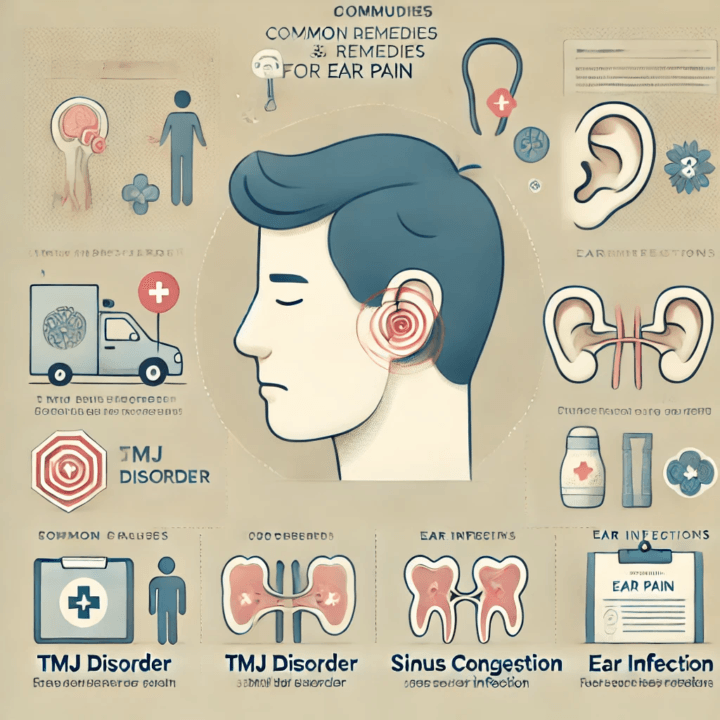
Managing the Meniere’s Tempest: Strategies for Control
I often tell people: while Meniere’s disease does not yet have a cure, we have plenty of ways to manage its symptoms, bringing a semblance of predictability back to life. My uncle, a long-haul truck driver who had to retire due to the unpredictable Meniere’s attacks, found that even small adjustments brought significant relief. He discovered a renewed sense of control.
Initial Responses to Meniere’s Symptoms
The first lines of defense frequently involve a combination of lifestyle adjustments and medication:
- Lifestyle Tweaks to Reduce Meniere’s Impact:
- Sodium Restriction: A low-sodium diet helps regulate fluid retention throughout the body, including the inner ear, potentially lessening the severity and frequency of Meniere’s disease episodes.
- Substance Moderation: Reducing caffeine and alcohol intake, alongside eliminating smoking, can considerably decrease symptom exacerbation.
- Stress Reduction: Becoming proficient in stress management techniques, like meditation or deep breathing exercises, can significantly influence the course of Meniere’s, as stress often acts as a potent trigger.
- Medication for Meniere’s Relief:
- Diuretics: These “water pills” help the body shed excess fluid, aiming to reduce the endolymphatic hydrops within the inner ear.
- Motion Sickness & Anti-Nausea Medications: Drugs such as meclizine or prochlorperazine effectively alleviate the intense vertigo, nausea, and vomiting that accompany acute Meniere’s attacks.
- Betahistine: While not FDA-approved in the U.S., this medication is commonly prescribed in many parts of the world, thought to improve blood flow in the inner ear or reduce vestibular nuclei activity.
When Symptoms Persist: Advanced Meniere’s Therapies
For those whose Meniere’s disease proves more resilient, additional interventions are available:
- Inner Ear Injections:
- Steroids: Medications like dexamethasone injected directly into the middle ear can calm inflammation and reduce vertigo, often with minimal risk to hearing.
- Gentamicin: This antibiotic, also delivered via injection into the middle ear, can selectively damage the balance-sensing hair cells, effectively controlling vertigo. However, it carries a known risk of further hearing loss, making its use a carefully considered decision.
- Rehabilitative Therapies & Devices:
- Vestibular Rehabilitation: Specific exercises, guided by a physical therapist, train the brain to compensate for inner ear dysfunction, enhancing balance and reducing the sensation of dizziness.
- Hearing Aids: For individuals experiencing progressive hearing loss with Meniere’s disease, hearing aids can significantly improve auditory function.
- Pressure Pulse Treatment: Devices like the Meniett pulse generator deliver gentle air pressure pulses to the middle ear, aiming to regulate inner ear fluid dynamics and alleviate Meniere’s symptoms.
Last Resorts: Surgical Options for Meniere’s Disease
In severe, intractable cases of Meniere’s disease, where all other treatments have failed to provide sufficient relief, surgical options become a consideration:
- Endolymphatic Sac Decompression: This procedure aims to alleviate pressure by draining excess fluid from the endolymphatic sac, often preserving hearing.
- Vestibular Nerve Section: By severing the vestibular nerve, balance signals from the affected ear are prevented from reaching the brain, effectively stopping vertigo attacks while striving to save hearing.
- Labyrinthectomy: This destructive procedure involves removing portions of the inner ear, typically reserved for cases where hearing in the affected ear is already severely compromised, as it results in complete hearing loss in that ear.
My friend, Sarah, initially resisted the idea of surgery, but after years of debilitating vertigo, she opted for a vestibular nerve section. “The silence from the spinning was a miracle,” she shared, “even with the adjustments that came after.” The choice of treatment for Meniere’s disease is highly personalized, a careful weighing of benefits and risks, always striving for improved quality of life.
Unresolved Questions: Debates Surrounding Meniere’s Disease
Meniere’s disease, for all our progress, remains shrouded in scientific debate, a testament to the intricate and often elusive nature of inner ear physiology. Experts frequently disagree on fundamental aspects, from its underlying causation to the most effective long-term strategies.
The Hydrops Conundrum
A central controversy revolves around endolymphatic hydrops: is this fluid buildup the primary cause of Meniere’s disease, or merely a symptom of a deeper, yet undiscovered, issue?
- Complex Presentation: We observe endolymphatic hydrops in individuals who never experience Meniere’s symptoms. Conversely, some diagnosed with Meniere’s disease do not consistently display hydrops when examined post-mortem or through imaging. This lack of perfect correlation begs the question of its precise role.
- Causality vs. Consequence: Some researchers hypothesize that hydrops might be a compensatory response to an initial, subtle inner ear injury, rather than the original instigator of the Meniere’s condition. This shift in perspective could redefine our therapeutic approaches.
Treatment Efficacy: A Scarcity of Definitive Proof
Another significant area of contention lies in the effectiveness of various Meniere’s disease treatments. Many widely accepted interventions lack the robust scientific validation of large-scale, double-blind, placebo-controlled studies, which are considered the gold standard for proving medical efficacy.
- Challenges in Research: The episodic and fluctuating nature of Meniere’s disease itself complicates research. Symptoms can naturally wax and wane, making it difficult to discern if improvement is due to a specific treatment, a placebo effect, or the disease’s natural course.
- Diets and Diuretics: While often recommended, the evidence supporting the long-term effectiveness of low-sodium diets and diuretics in consistently reducing Meniere’s disease symptoms is surprisingly limited, leading to ongoing discussion about their true impact.
- Surgical Nuances: Even surgical procedures, such as endolymphatic sac decompression, despite showing high vertigo control rates, continue to fuel debate among specialists concerning their exact mechanism and optimal application. The difficulty of conducting blinded trials for surgical interventions means much evidence remains observational or anecdotal.
This ongoing discourse underscores Meniere’s disease as a condition still ripe for discovery, where new insights could fundamentally reshape our understanding and management paradigms. The scientific community continues its quest for clearer answers, acknowledging the current landscape of uncertainties.
New Horizons: Advances in Meniere’s Disease Research
The future for Meniere’s disease management and understanding appears increasingly bright, thanks to relentless scientific pursuit. Researchers across the globe are pushing boundaries, generating promising advancements that promise to improve both diagnosis and treatment for those living with Meniere’s disease.
Smarter Diagnostics: Seeing the Unseen
Our ability to accurately identify Meniere’s disease is rapidly evolving:
- Advanced MRI Techniques: Modern MRI protocols now enable physicians to directly visualize endolymphatic hydrops within the inner ear of living patients. This capability moves Meniere’s diagnosis beyond purely clinical symptoms, allowing for objective confirmation of the fluid imbalance. This precision means better-targeted Meniere’s treatment planning.
- Optical Coherence Tomography (OCT): Imagine a handheld device that allows a clinician to peer directly into the inner ear in a clinic setting. That’s the promise of OCT. This technology is, for the first time, studying the human inner ear in real-time, offering unprecedented insights into conditions like Meniere’s disease and potentially revolutionizing point-of-care diagnosis and monitoring.
Next-Generation Treatments: Beyond Symptom Management
The development pipeline for new Meniere’s disease therapies is robust:
- SPI-1005 (Ebselen): A novel anti-inflammatory compound, SPI-1005, has shown remarkable results in clinical trials. This oral capsule, containing ebselen, works by mimicking an important enzyme, glutathione peroxidase (GPx), which helps reduce neuroinflammation throughout the nervous system, including the inner ear. Early findings suggest it improves hearing loss and speech discrimination in Meniere’s patients, offering a new pathway for relief.
- Migraine-Targeted Therapies: Given the observed overlap between Meniere’s disease and vestibular migraines, scientists are exploring medications that specifically target molecular pathways associated with migraines. This approach recognizes shared mechanisms and broadens the therapeutic arsenal for Meniere’s disease.
- Sustained-Release Steroids: Imagine a single ear injection that provides weeks of continuous relief. Sustained-release steroid gels, such as SPT-2101, are being trialed to deliver a steady, localized dose of anti-inflammatory medication directly to the inner ear, reducing vertigo days for Meniere’s patients for extended periods.
- Gene Therapy: Perhaps the most groundbreaking advancement on the horizon is gene therapy. Already seeing international adoption for certain types of hearing loss, this technology holds immense potential to address Meniere’s disease at a fundamental genetic level in the coming years, offering hope for a curative intervention.
Emerging Theories: Rethinking the Disease
New concepts are challenging long-held beliefs, prompting a re-evaluation of Meniere’s disease pathophysiology:
- Hydrops as a Response: Some theories now propose that endolymphatic hydrops may not be the initial problem but rather a secondary, compensatory response to an earlier, subtle injury within the inner ear. This changes the understanding of disease progression.
- Otoconia and Obstruction: One intriguing theory suggests that dislodged microscopic crystals (otoconia) from the saccule could physically obstruct narrow ducts in the inner ear, leading to the fluid imbalances characteristic of Meniere’s disease. This draws parallels to benign paroxysmal positional vertigo (BPPV).
- Immune System Involvement: An increased understanding of the immune system’s role within the endolymphatic sac suggests that immune stimulation or dysfunction could disrupt fluid regulation, leading to hydrops and driving Meniere’s symptoms.
These diverse research avenues underscore a collective, global effort to demystify Meniere’s disease. With improved diagnostic capabilities, innovative Meniere’s treatment strategies, and a deeper grasp of its underlying mechanisms, the future promises a more predictable, less debilitating existence for those facing this challenging condition.
Living Unspun: Navigating Meniere’s Disease
Meniere’s disease can be profoundly challenging. Its unpredictable attacks often impact every facet of life, from the simple act of driving to a person’s overall mental well-being. This is precisely why integrating counseling and stress management into a Meniere’s disease management plan becomes so critically important. I have witnessed firsthand the profound relief individuals experience when they learn effective coping mechanisms, realizing they are not alone in their struggle.
- Testimonial: “I used to dread leaving the house,” confided one person I spoke with, “the sudden dizziness, the fear of falling. But with proper support and learning to manage my stress, my world began to open up again. It is a slow climb, but I am making progress, moving forward one steady step at a time.”
While Meniere’s disease can, over time, lead to permanent hearing loss, and some degree of residual imbalance might linger even as vertigo attacks subside, the current landscape offers considerable hope. Ongoing research, fueled by diagnostic advancements and innovative therapies, paints a picture of a more manageable future for those living with this condition. Each scientific breakthrough, each new understanding, contributes to a collective effort toward providing greater stability and improved quality of life. The journey with Meniere’s disease is undeniably tough, yet the horizon shows clear signs of progress, promising a path toward living a life less defined by its unpredictable spins.












Post Comment