The Itch You Can’t Scratch: A Deep Dive into Pruritus (and How We’re Finally Getting Smarter About It!)
Table of Contents

The Itch You Can’t Scratch: A Deep Dive into Pruritus (and How We’re Finally Getting Smarter About It!)
Itching is a universal experience, from a fleeting annoyance caused by a mosquito bite to a persistent, maddening sensation that can disrupt daily life. While often dismissed as a minor irritation, chronic itching, known medically as pruritus, is a complex condition that warrants serious attention. For centuries, understanding and treating the persistent urge to scratch has presented a significant challenge. However, thanks to ongoing research and new discoveries, our approach to managing this uncomfortable sensation is evolving, offering more targeted and effective solutions than ever before.
The Annoying Sensation of Pruritus
Most people associate itching with something obvious, like a bug bite or dry skin. But pruritus, the medical term for itching, is far more intricate. It’s that compelling urge to scratch, and it can affect a small area or spread across the entire body. Sometimes, it appears with a visible rash; other times, the skin looks completely normal, adding to the mystery.
Beyond the common culprits like overly dry skin, allergic reactions, or inflammatory conditions such as eczema (atopic dermatitis), persistent itching can sometimes signal an underlying health issue. Problems with organs like the liver or kidneys, thyroid imbalances, or even certain medications can trigger widespread itching. Nerve damage, as seen in conditions like shingles, or even ongoing stress, can also play a significant role. The diverse origins of itching highlight why a thorough investigation is often necessary to find relief.
The symptoms of pruritus vary widely. You might experience redness, dry patches, bumps, or full-blown rashes. In severe cases, constant scratching can lead to broken skin, bleeding, thickened skin, and even infections. If itching lasts for more than six weeks, it’s considered chronic pruritus. This prolonged discomfort can severely impact sleep, concentration, and overall well-being, diminishing a person’s quality of life. Understanding these varied manifestations and potential causes is the first step toward effective management.
A Historical Look at Itch Remedies
Humanity’s struggle with itching is not new. Our ancestors employed a range of fascinating, if sometimes unusual, methods to find relief. Ancient Egyptians, as far back as 3,000 years ago, used compresses made from beans and onions, or mixtures of milk and sea salt, to “still” itchy skin. The Romans valued hygiene, using public baths and body oils to moisturize and calm skin discomfort. Moving into the Byzantine era, physicians like Alexander of Tralles suggested crushed rue and alum mixed with honey for an itchy scalp. Even more strikingly, Greek physician Paul of Aegina in the 7th century listed squill, metallic components, and goat droppings for external application against itch. Meanwhile, traditional Chinese medicine has a long history of addressing conditions like infantile eczema with herbal remedies and practices like acupuncture.
During the Middle Ages, treatments blended faith, folk traditions, and herbal knowledge. Herbal baths made from plants like sage, thyme, and chamomile were common. Honey was prized for its protective qualities, and animal fats provided moisture for dry skin. Yet, during the European Renaissance, some doctors believed that skin conditions like oozing eczema were the body’s way of expelling toxins, leading to advice that often discouraged treatment.
The scientific understanding of skin conditions began to formalize in the 19th century. In 1818, English physicians Willan and Bateman coined the term “eczema.” This period saw the introduction of topical remedies like tar and sulfur, along with recommendations for lukewarm baths and emollients (moisturizers). It was also the era of “patent medicines”—over-the-counter concoctions, some of which, like Mentholatum, found lasting popularity. The 20th century brought significant medical advancements, including the widespread use of topical corticosteroids in the 1950s. Antihistamines also became popular for itch relief, though their effectiveness for many chronic forms of itching was often linked more to their sedative effects than to directly addressing the itch itself.
Modern Medical Perspectives on Itching
Today, medical professionals recognize that effective itch relief depends on identifying and addressing its root cause. Itching is rarely a simple symptom; it often involves a complex interplay of skin conditions, internal medical issues, nerve problems, or even psychological factors. This nuanced understanding has shifted the focus from merely suppressing the itch to a more comprehensive approach.
Becoming an “itch detective” involves a detailed assessment. Doctors typically start with a thorough physical examination and a discussion about the nature of your itch, including its severity, patterns, and any associated factors. If an underlying internal condition is suspected, blood tests may be ordered to check liver and kidney function, thyroid levels, or blood counts. In some cases, imaging studies might be recommended to investigate deeper systemic issues. Careful observation of the skin for specific lesions versus secondary damage from scratching also guides diagnosis.
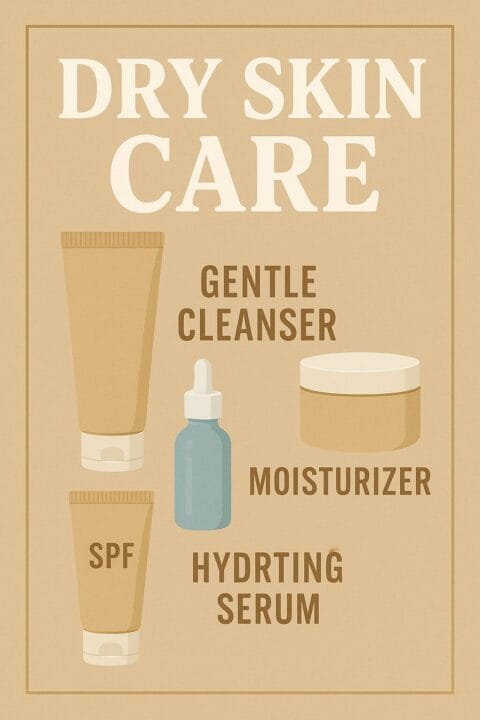
Beyond prescribed medications, everyday self-care remains a cornerstone of itch management. Doctors strongly recommend using fragrance-free moisturizers regularly, especially after bathing, to maintain skin hydration. Taking cool or lukewarm baths, possibly with soothing additives like colloidal oatmeal or Epsom salts, can also provide relief. Identifying and avoiding triggers such as harsh soaps, scratchy fabrics like wool, or specific allergens is crucial.
Breaking the “itch-scratch cycle” is essential but challenging. Scratching provides temporary relief but ultimately worsens the itch and can lead to skin damage and infection. Medical advice emphasizes keeping nails short and clean, applying cool compresses, or gently tapping the itchy area instead of scratching. The mind-body connection is also increasingly recognized; stress and anxiety can intensify itching, so practices like meditation, yoga, or counseling can be valuable components of a treatment plan.
It’s important to know when to seek professional help. If your itch is severe, widespread, unexplained, or interferes significantly with your daily life or sleep, a visit to a doctor or dermatologist is advisable. Also, if itching is accompanied by other concerning symptoms like unexplained weight loss, fever, or night sweats, prompt medical evaluation is necessary.
Addressing Common Itch Myths and Unanswered Questions
Despite advancements, several myths and ongoing questions surround the phenomenon of itching, especially chronic pruritus.
One persistent misconception is that eczema is contagious. In reality, eczema is a genetic condition influenced by internal factors and cannot be “caught” from another person. While it can flare up on different parts of an individual’s body, it does not spread like an infection. Similarly, the advice to “just don’t scratch” is overly simplistic. While scratching undeniably aggravates the skin and worsens symptoms, simply refraining from scratching isn’t a cure for a chronic condition. Moreover, unconscious scratching during sleep is common and difficult to control.
Chronic itching is far from a “minor” issue. Its debilitating effects on sleep, mental health (leading to anxiety and depression), and overall quality of life are well-documented. It can impair concentration and disrupt daily routines, making it a significant health concern that demands effective treatment.
A key debate in treatment involves the limited effectiveness of traditional antihistamines for many types of chronic itch. This is because many forms of pruritus are not primarily driven by histamine, but rather by a complex network of other signaling molecules and nerve pathways. This realization has shifted research toward more targeted therapies. The definition of “treatment success” is also being re-evaluated. While reducing itch from a severe level to a moderate one might seem like an improvement, current understanding suggests that even a small amount of residual itch can significantly impact a patient’s quality of life. The goal is now often complete or near-complete relief.
For too long, itch was viewed merely as a symptom of another condition. However, it is now increasingly recognized as a complex phenomenon with its own distinct mechanisms, involving intricate interactions between skin cells, immune cells, the nervous system, and the brain. This recognition is crucial for driving dedicated research into better solutions. Furthermore, a growing understanding of the “brain-skin connection” highlights the significant role the nervous system plays in chronic itch, often independent of visible inflammation. It’s not always just a skin problem; sometimes, it’s a nerve problem.
The Future of Itch Management: Innovative Treatments
The landscape of itch treatment is undergoing a revolutionary transformation, moving away from general approaches toward highly specific, precision medicine. The goal is to develop therapies that target the exact molecules and pathways responsible for chronic itching, offering rapid and sustained relief.
One of the most promising areas is biologic therapies. These advanced drugs target specific immune signals that trigger inflammation and itch. For instance, medications like dupilumab are already approved for conditions like eczema and prurigo nodularis, working by blocking key immune pathways (IL-4 and IL-13). Another exciting biologic, nemolizumab, is being explored for its ability to target IL-31, another crucial itch-driving signal. These treatments represent a significant leap forward, directly addressing the underlying immune dysregulation.
JAK inhibitors are another class of innovative treatments. Available as both pills and creams, these small molecules interrupt a critical signaling pathway involved in various inflammatory conditions. They are showing immense promise for providing quick itch relief, even in cases where the cause of itching is unclear. They represent a versatile option for many forms of chronic pruritus.
Surprisingly, some new drugs are modulating the body’s opioid receptors. While these receptors are traditionally associated with pain, certain types are also involved in transmitting itch signals. For example, difelikefalin is already approved for itching linked to kidney disease, working by selectively targeting kappa-opioid receptors to calm itch sensations without significant central nervous system effects.
Beyond these major advancements, researchers are exploring a wide array of other therapeutic avenues. This includes blocking “Substance P,” a neuropeptide that plays a role in provoking itch, and investigating the impact of the gut microbiome on skin health. Specialized compounded creams, sometimes containing ingredients like ketamine, amitriptyline, and lidocaine, are also being used to target nerve-related itching. The overarching trend is towards treatments that directly intervene in the complex nerve pathways that cause the sensation of itch.
The future of itch relief is bright, with many of these novel therapies designed for rapid action. This shift promises not just to manage but to significantly reduce or even eliminate chronic itching, offering a new sense of hope for the millions who suffer daily from this challenging condition.
For more information on clinical research trials, visit : NIH Clinical Research Trials












Post Comment