Anti-Inflammatory Foods: Your Plate for Less Pain and Better Health
Table of Contents
Anti-Inflammatory Foods: Your Plate for Less Pain and Better Health
Anti-inflammatory foods are revolutionizing how we approach persistent discomfort and the silent battles within our bodies. I recall a time, not so long ago, when persistent aches often seemed an unavoidable aspect of life, a condition one simply endured. We often overlook the silent operations within our physiology, perceiving symptoms as isolated events rather than manifestations of deeper systemic processes. Consider inflammation: a crucial biological alarm, signaling repair when a cut appears or an infection takes hold. This acute response, a localized crimson warmth, swelling, and temporary pain, marks a salutary effort to restore equilibrium. However, the contemporary landscape reveals a more insidious antagonist—chronic inflammation, a smoldering, protracted physiological state, less overtly dramatic than its acute counterpart yet profoundly detrimental. This persistent, low-grade internal agitation, if permitted to endure, fuels conditions ranging from cardiovascular pathologies and arthritic degeneration to neurodegenerative disorders like Alzheimer’s. The crucial question, then, becomes: what role does our daily sustenance play in this intricate dance of cellular harmony and discord? Our dietary choices, often underestimated in their profound influence, act as either potent incendiaries, stoking the fires of this ceaseless internal conflagration, or as sophisticated fire suppressants, diligently working to extinguish these metabolic embers.
Understanding Inflammation: The Body’s Silent Alarm and Persistent Foe
Our physiological apparatus possesses an intricate defense mechanism, inflammation, a fundamental response to injury or infection. Initially, this process is unequivocally beneficial; imagine a simple cut on your finger. Within moments, your body dispatches a complex array of cellular and molecular agents to the site, initiating repair, halting pathogens, and preventing further damage. This acute, short-term inflammation is a testament to our inherent capacity for self-preservation. It is a rapid, protective physiological event.
Yet, beyond the immediate efficacy of acute inflammation lies a pervasive, less evident, but profoundly more dangerous condition: chronic inflammation. This persistent state, often asymptomatic in its early stages, subtly undermines health, eroding tissues and organs over extended periods. Factors as diverse as environmental toxins, sustained psychological stress, inadequate restorative sleep, the inexorable march of age, immune system dysregulation, and, crucially, our daily caloric intake collectively contribute to this enduring inflammatory burden. What sort of health implications might such a prolonged internal skirmish engender? The consequences are far-reaching:
- Heart Disease: Chronic inflammation accelerates arterial plaque buildup, a precursor to cardiac events.
- Arthritis: Joint pain and degeneration often trace their origins to prolonged inflammatory responses.
- Type 2 Diabetes: Persistent inflammation contributes to insulin resistance, making blood sugar regulation a formidable challenge.
- Cancer: Inflammatory environments provide fertile ground for abnormal cellular proliferation and tumor progression.
- Alzheimer’s Disease: Mounting evidence suggests neuroinflammation plays a significant part in the pathogenesis of cognitive decline.
- Autoimmune Conditions: When the immune system mistakenly targets healthy tissues, chronic inflammation becomes a central feature.
My point is this: we possess agency over a significant contributor to chronic inflammation—our diet. Certain foods, by virtue of their biochemical composition, either exacerbate or ameliorate this internal strife. The deliberate selection of anti-inflammatory foods thus becomes not merely a dietary preference, but a strategic health imperative, offering a potent, accessible tool in the sustained pursuit of vitality and freedom from persistent systemic irritation.
Historical Resonance and Modern Research on Anti-Inflammatory Eating
The notion that sustenance influences well-being, particularly regarding inflammatory conditions, is hardly a modern revelation. Indeed, this wisdom echoes through the corridors of ancient civilizations. Hippocrates, around 400 B.C., a foundational figure in Western medicine, articulated a philosophy startlingly resonant with contemporary thought: “Let food be thy medicine and medicine be thy food.” This isn’t just a poetic adage; it reflects a deep, intuitive recognition among ancient Greeks, as well as practitioners of Ayurveda in India and Traditional Chinese Medicine, that dietary choices possessed profound therapeutic capacities. They observed, without the benefit of our current molecular tools, the direct impact of specific plants, herbs, and spices on the body’s internal balance and healing processes.
However, the scientific validation of these ancient insights required a considerable chronological leap. The true genesis of our modern understanding concerning the anti-inflammatory properties of food began to consolidate in the 1970s. During this period, pioneering researchers initiated serious investigations into the intricate links between dietary patterns and the emergence of chronic diseases. A significant breakthrough involved the identification of C-reactive protein (CRP) as a quantifiable biomarker, an invaluable indicator of systemic inflammation within the blood. The measurement of CRP allowed scientists to move beyond observation, offering a tangible metric to correlate diet with inflammatory load.
The 1990s witnessed the popularization of the anti-inflammatory diet concept, championed by influential figures who bridged the gap between complex biochemistry and public health. Biochemist Dr. Barry Sears, through his work on The Zone Diet, illuminated the role of specific macronutrient ratios in controlling diet-induced inflammation. His research emphasized omega-3 fatty acids and polyphenols for maintaining hormonal balance, a crucial factor in modulating inflammatory responses. Simultaneously, Dr. Andrew Weil, a leading proponent of integrative medicine, introduced his widely recognized “anti-inflammatory food pyramid.” This model, synthesizing nutritional science with principles from traditional Mediterranean and Asian eating patterns, underscored the importance of whole, unprocessed foods and healthy fats in mitigating systemic inflammation. These figures, each in their own way, laid the groundwork for a public health paradigm shift, where selecting anti-inflammatory foods transitioned from ancient lore to actionable, evidence-supported dietary guidance.
Building Your Anti-Inflammatory Plate: Foods to Prioritize and Limit
Constructing a diet focused on reducing inflammation often feels like a puzzle, but some established dietary patterns already offer clear blueprints. The Mediterranean diet and the DASH (Dietary Approaches to Stop Hypertension) diet stand as exemplars, consistently lauded by scientific consensus for their inherent anti-inflammatory properties. These eating styles fundamentally prioritize a bounty of plant-based foods, healthy fats, and lean proteins, naturally discouraging many of the pro-inflammatory culprits prevalent in modern eating habits.
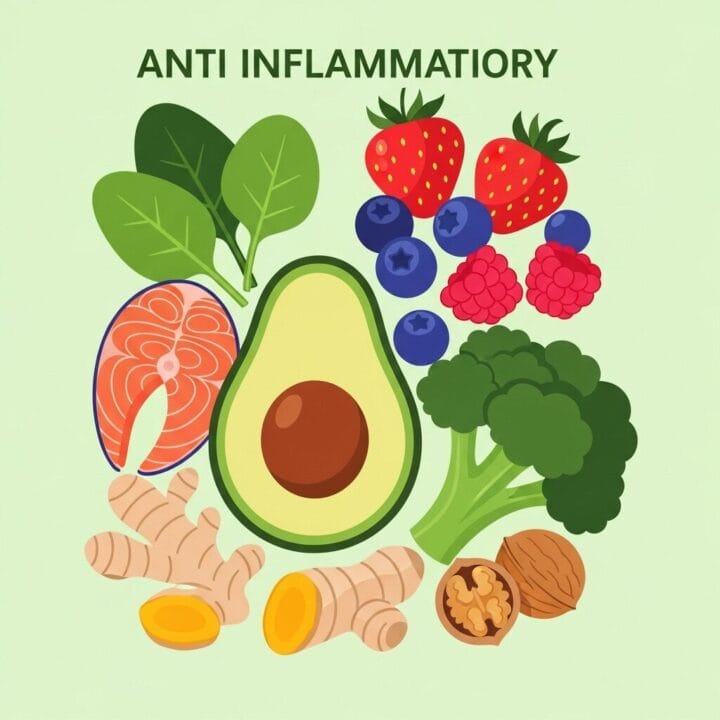
What, then, are the star players in the anti-inflammatory food league? Here’s my concise rundown of what you should be piling on your plate to truly impact your internal environment:
- Oily Fish: Think salmon, mackerel, sardines, and anchovies. These are rich in omega-3 fatty acids, powerful inflammation fighters that reduce C-reactive protein (CRP) levels.
- Vibrant Berries: Blueberries, raspberries, blackberries, and strawberries. They are bursting with anthocyanins, compounds that actively inhibit inflammatory pathways.
- Turmeric with Black Pepper: The golden spice contains curcumin, an potent anti-inflammatory agent. Crucially, combine it with a pinch of black pepper, which contains piperine to dramatically enhance curcumin absorption.
- Power-Packed Avocados: Loaded with monounsaturated fatty acids (MUFAs), vitamins C and E, fiber, and potassium. Avocados help control oxidative stress and reduce inflammation.
- Extra Virgin Olive Oil (EVOO): A cornerstone of the Mediterranean diet. EVOO contains oleocanthal, a compound with anti-inflammatory effects akin to ibuprofen.
- Dark Leafy Greens: Spinach, kale, Swiss chard, arugula. These vegetables are nutritional powerhouses, dense in vitamins, minerals, and antioxidants that actively fight inflammation.
- Walnuts: Among the best nuts for inflammation, offering a good source of omega-3s and antioxidants.
- Green Tea: Contains catechins, powerful antioxidants with well-documented anti-inflammatory properties.
- Onions and Garlic: These common kitchen staples are packed with anti-inflammatory compounds.
- Beets: Their vibrant color comes from betanin, a pigment with anti-inflammatory effects.
- Bell Peppers: Rich in vitamin C and antioxidants like quercetin and ferulic acid, they combat inflammation effectively.
On the flip side, some foods act as party poopers, actively stoking the inflammatory fires. For anyone serious about controlling inflammation, I suggest a radical reduction, if not outright elimination, of these items:
- Processed Junk Foods: Anything heavily refined, packaged, and devoid of whole, natural ingredients.
- Sugary Drinks and Refined Sugars: Sodas, fruit juices (often concentrated), candies, and desserts. These cause rapid blood sugar spikes, which fuel inflammation.
- Refined Carbohydrates: White bread, white pasta, pastries, and many breakfast cereals. These convert quickly to sugar, contributing to inflammatory responses.
- Trans Fats: Often found in fried foods, commercial baked goods, and some margarines. These are notorious for increasing systemic inflammation.
- Excessive Red and Processed Meats: Hot dogs, bacon, deli meats, and large quantities of red meat. Their consumption is consistently linked to higher inflammatory markers.
- Certain Seed Oils: Soybean, corn, sunflower, safflower, grapeseed oils, when consumed in disproportionately high amounts compared to omega-3s, can promote inflammation.
I had a client, let’s call him Mark, a construction worker, suffering from chronic joint pain that he blamed on his physical job. His diet was full of fried foods, sugary sodas, and processed lunch meats. We switched him to lunches packed with salmon salads on whole-grain bread, snacking on walnuts and berries, and replacing sodas with green tea. Within three months, his reported pain decreased significantly, and he moved with greater ease. He told me, “I just feel… lighter. Like my body isn’t fighting itself anymore.” That’s the power of these anti-inflammatory foods at work. This isn’t about deprivation; it is about strategic substitution for real, tangible results.
Navigating the Anti-Inflammatory Food Debates: Separating Fact from Fiction
The landscape of dietary advice can often feel like a minefield of conflicting information, and anti-inflammatory eating is no exception. With so much chatter online, it is easy to get caught in loops of misinformation. What should you actually believe when it comes to specific foods and inflammation? Let me clear the air on some common points of contention, often amplified by social media trends that sometimes promote overly restrictive approaches without robust scientific backing.
First, let’s talk about dairy. Is it good or bad for inflammation? For years, I heard conflicting messages, with some online gurus advocating for its complete removal. However, a significant body of research indicates that for the vast majority of people, dairy products are either neutral or even have an anti-inflammatory effect. Unless you possess a diagnosed dairy allergy or lactose intolerance, there is little scientific reason to eliminate nutrient-rich dairy from your diet for inflammation reduction. The key here, as with many food groups, lies in individual response and ensuring you do not have a specific sensitivity.
Next, the nightshade vegetables—tomatoes, potatoes, eggplants, and peppers. A persistent myth claims these vegetables inherently cause inflammation due to compounds like solanine. This idea, lacking credible human research, often leads to unnecessary avoidance of highly nutritious foods. In reality, nightshades are rich in antioxidants, vitamins, and minerals that combat inflammation. For instance, tomatoes, often maligned, contain lycopene, a potent antioxidant. I say, unless you personally experience a noticeable adverse reaction, keep these colorful powerhouses on your plate.
The digital space often buzzes with extreme claims promising “cure-all” solutions through drastic dietary restrictions—cutting out all gluten, sugar, or even foods containing lectins. While excessive added sugar and trans fats are indeed pro-inflammatory, the idea that everyone must eliminate gluten or dairy without a specific diagnosis (like celiac disease or a verified sensitivity) is simply unfounded. In fact, many whole grains, which contain gluten, are rich in fiber and beneficial compounds that support anti-inflammatory processes. Lectin-containing foods, such as beans and grains, when properly prepared (e.g., cooked thoroughly), offer vital fiber and nutrients that contribute to a healthy, diverse gut microbiome, a crucial player in inflammation regulation.
This highlights a critical distinction: an anti-inflammatory diet supports medical treatment; it does not replace it. It is a powerful adjunctive strategy, not a magic bullet. Be cautious of any voice promising a complete “cure” for complex conditions solely through diet. My philosophy is always one of addition rather than radical subtraction—focus on incorporating more anti-inflammatory foods rather than obsessively eliminating broad categories without sound reasons. For individuals on a tight budget, the perceived expense of fresh produce can be a barrier. However, emphasizing seasonal vegetables, frozen fruits and vegetables, and affordable staples like beans and lentils can make an anti-inflammatory diet accessible to more people.
The Future of Anti-Inflammatory Eating: Personalized Plates and Precision Nutrition
We stand at the precipice of a revolution in dietary science, one that promises to render generic nutritional advice obsolete. The future of anti-inflammatory eating is moving with astounding velocity toward personalized nutrition, where our plates will be sculpted not by broad guidelines, but by the intricate blueprint of our individual biological identities. Think about it: a diet precisely engineered for your unique genetic code, your specific gut microbial composition, and your body’s nuanced inflammatory triggers. This isn’t science fiction; it is the trajectory of current research.
How will this transformation manifest?
- AI-Driven Dietary Blueprints: Imagine artificial intelligence analyzing vast datasets, integrating your genomics, metabolomics, and the unique bacterial symphony within your gut. This “foodome” project is already cataloging tens of thousands of food molecules, aiming to build a comprehensive atlas of diet-body interactions. This analytical prowess will not just identify which anti-inflammatory foods work for you, but why and how. Companies are already leveraging AI to customize functional foods, precisely targeting individual needs for enhanced gut health, immunity, or cognitive function.
- The Unveiling of Novel Bioactive Compounds: Scientists are ceaselessly exploring “nutritional dark matter”—the myriad uncharted compounds within foods. We are discovering new anti-inflammatory agents in unexpected places:
- Plant-derived peptides: Found in legumes like soybeans and beans, these small protein fragments show immense promise in modulating pro-inflammatory molecules like eicosanoids and cytokines.
- Marine bioactives: From algae polyphenols to sulfated polysaccharides, the ocean’s depths hold untapped resources for potent anti-inflammatory properties.
- Advanced fermentation: This ancient technique, now supercharged by biotechnology, is creating “Fermbiotics”—fermented products with enhanced anti-inflammatory characteristics, ready for incorporation into diverse food products and supplements.
- The Gut Microbiome as Center Stage: We are rapidly appreciating the profound influence of our gut bacteria on systemic inflammation. Future strategies will intensify focus on nurturing a diverse and beneficial gut microbiota through:
- Targeted prebiotics: Specific fibers designed to feed beneficial bacteria that produce anti-inflammatory short-chain fatty acids.
- Precision probiotics: Not just general probiotic supplements, but strains meticulously selected for their ability to modulate inflammatory pathways within your unique gut ecosystem.
- Fermented foods like kimchi, kefir, and certain yogurts, rich in these beneficial microorganisms, will play an even more prominent role.
- Holistic Integration: While food remains foundational, the future recognizes that inflammation is a multi-factorial phenomenon. Expect increasingly integrated approaches that weave personalized nutrition with equally critical lifestyle elements:
- Optimized Sleep: Chronic sleep deprivation is a known inflammatory trigger.
- Stress Management Protocols: Sustained psychological stress profoundly impacts inflammatory markers.
- Tailored Exercise Regimens: Physical activity, when appropriate, is a potent anti-inflammatory intervention.
The era of one-size-fits-all diet plans is gracefully receding. The emerging paradigm, steeped in scientific precision and individualized data, promises a far more effective and satisfying path toward mitigating inflammation and fostering enduring health. This means we will be better equipped to harness the true potential of anti-inflammatory foods as personalized medicine.
Boosting Your Anti-Inflammatory Lifestyle: Practical Strategies for Daily Life
Implementing an anti-inflammatory eating pattern does not demand a complete overhaul overnight; instead, it flourishes through consistent, strategic adjustments. My experience shows that making manageable changes leads to lasting habits. How, then, might you practically integrate more anti-inflammatory foods into your daily routine and truly impact your health? Let me share some actionable steps:
- Strategic Swaps in Your Kitchen:
- Replace refined grains (white bread, white pasta) with whole grains like quinoa, brown rice, whole wheat pasta, or oats. My preference: a robust quinoa salad packed with colorful vegetables makes a fantastic, filling lunch.
- Opt for healthy fats. Ditch the highly processed vegetable oils high in omega-6s. Instead, embrace extra virgin olive oil for cooking and dressings, and integrate avocados and nuts like walnuts and almonds into snacks.
- Choose lean protein sources. Prioritize fatty fish (salmon, sardines) a few times a week. Incorporate plant-based proteins such as lentils, beans, and tofu frequently. Reduce reliance on red and processed meats.
- Embrace the Spectrum of Produce:
- Fill half your plate with vegetables. Focus on dark leafy greens (spinach, kale), vibrant berries, bell peppers, broccoli, and other cruciferous vegetables. Buy frozen options to save money and ensure year-round availability.
- Snack on fruits. Berries, cherries, and citrus fruits are packed with antioxidants. A handful of blueberries is a simple, effective anti-inflammatory snack.
- Spices and Herbs Are Your Allies:
- Use turmeric liberally. Remember the power duo: combine turmeric with black pepper in curries, soups, or even smoothies for maximum benefit.
- Integrate ginger and garlic. These potent spices add incredible flavor while delivering significant anti-inflammatory compounds. Fresh ginger in tea or stir-fries is an easy win.
- Experiment with cinnamon, rosemary, and oregano—all boast beneficial properties.
- Hydration Matters:
- Swap sugary drinks for water or green tea. Green tea, in particular, offers powerful catechins that reduce inflammation. This single swap can dramatically cut down on inflammatory sugar intake.
- Smart Cooking Methods:
- Prefer baking, steaming, or light stir-frying. Avoid deep-frying or high-heat grilling, especially for meats, as these methods can generate pro-inflammatory compounds.
- Address Affordability:
- Shop smart. Look for sales on fresh produce, buy in-season, and leverage frozen fruits and vegetables. Dried beans and lentils are incredibly inexpensive and nutrient-dense. This approach ensures an anti-inflammatory diet remains accessible, not an exclusive club.
I often remind people that this isn’t about perfection; it is about consistency. Small, daily choices accumulate into significant health dividends. Start with one or two changes, like swapping your morning bagel for oatmeal with berries and walnuts, or replacing a soda with green tea. These incremental shifts can dramatically alter your body’s internal inflammatory environment.
How My Plate Changed: A Personal Story about Anti-Inflammatory Eating
I remember my early thirties; I felt perpetually worn down. My knees ached after a run, my skin often felt irritated, and my general energy levels were consistently low. I attributed it to stress, to getting older, to anything but what I put on my plate every single day. My diet, honestly, was a typical American one: lots of processed snacks, red meat several times a week, sugary coffee, and an unfortunate reliance on takeout. I had heard about anti-inflammatory foods, but it sounded like another restrictive diet fad, frankly.
My turning point arrived when a friend, a physician, gently pointed out my reliance on over-the-counter pain relievers. “What if you tried to fix the cause, not just the symptom?” she asked. That question resonated. It wasn’t about a cure-all, but about support. I started small, cutting out the daily sugary soda, replacing it with water infused with lemon and ginger. Then, I added a handful of walnuts and blueberries to my breakfast.
The initial weeks were interesting. I felt more energetic, less sluggish. My knee pain, while not vanishing, became less constant, less insistent. The real shift came when I started integrating fatty fish like salmon into my week and drastically cut back on processed meats. Cooking became an experiment. I experimented with generous amounts of turmeric and black pepper in my stir-fries, I made massive salads packed with colorful bell peppers and dark leafy greens dressed simply with extra virgin olive oil. My taste buds adjusted, began to crave the vibrancy of these natural ingredients.
After six months, the transformation was undeniable. My skin had cleared, my joint discomfort was minimal even after intense workouts, and my energy levels were consistently high. I even noticed my focus at work improved. It was not a magical overnight fix; it was a gradual, consistent effort. This approach taught me that nourishing my body with anti-inflammatory foods wasn’t a punishment, but a profound act of self-care. My experience wasn’t unique; it was simply a testament to what happens when you consciously choose to reduce the internal battle and fuel your body’s natural healing processes.
Conclusion: Fueling Your Body with Anti-Inflammatory Foods
The journey towards reduced inflammation and enhanced vitality begins with the deliberate choices we make at every meal. What we consume transcends mere caloric intake, serving as either a catalyst for cellular stress or a profound source of physiological restoration. We have explored the critical distinction between acute, beneficial inflammation and its chronic, insidious counterpart, tracing how the latter contributes to an array of debilitating conditions from heart disease to neurodegenerative disorders. History shows us that sages understood food as medicine, a wisdom now validated by modern scientific inquiry, which systematically identifies specific compounds and dietary patterns capable of modulating inflammatory responses.
By prioritizing a plate rich in omega-3 fatty acids from oily fish, a rainbow of berries and dark leafy greens, the golden potency of turmeric, and the wholesome goodness of extra virgin olive oil, we actively equip our bodies to quell internal fires. Simultaneously, judiciously limiting processed foods, refined sugars, trans fats, and excessive red meats becomes a strategic retreat from the drivers of chronic systemic agitation. While debates persist and individual sensitivities demand attention, the overarching consensus champions an eating style rooted in whole, unprocessed anti-inflammatory foods—a testament to the enduring power of mindful nourishment. The future promises personalized approaches, leveraging cutting-edge science to tailor dietary interventions to our unique biological profiles, further enhancing our capacity to mitigate inflammation. For now, embracing these principles empowers us to reclaim comfort, sharpen our minds, and bolster our overall health, one deliberate choice at a time. Therefore, actively choosing anti-inflammatory foods is a foundational pillar for a healthier future.
Frequently Asked Questions about Anti-Inflammatory Foods
Q1: What exactly is inflammation, and why should I care about anti-inflammatory foods?
A1: Inflammation is your body’s natural response to injury or infection. Acute inflammation helps heal, but chronic, long-term inflammation contributes to serious conditions like heart disease, arthritis, and diabetes. Focusing on anti-inflammatory foods helps reduce this harmful chronic state, promoting better overall health.
Q2: Which anti-inflammatory foods should I add to my diet first?
A2: I suggest starting with oily fish like salmon for omega-3s, a variety of berries, dark leafy greens such as spinach and kale, and incorporating spices like turmeric (with black pepper) and ginger. Extra virgin olive oil is also an excellent choice for cooking and dressings. These are powerful anti-inflammatory foods.
Q3: Are there any common foods that people think are inflammatory but are actually good?
A3: Absolutely. Nightshade vegetables (like tomatoes, bell peppers, potatoes, eggplant) are often mistakenly believed to cause inflammation, but they are rich in beneficial antioxidants. Dairy, for most people without a specific intolerance, also tends to be neutral or even anti-inflammatory. These can be valuable anti-inflammatory foods.
Q4: How quickly can I expect to see results from an anti-inflammatory diet?
A4: Results vary by individual, but many people report feeling more energetic and experiencing reduced aches within a few weeks to a few months of consistently incorporating anti-inflammatory foods and limiting pro-inflammatory ones. It is a long-term strategy for sustained wellness.
Q5: Is an anti-inflammatory diet a cure for chronic conditions like arthritis?
A5: An anti-inflammatory diet is a powerful supportive strategy that can significantly reduce symptoms and improve quality of life for many chronic conditions, including arthritis. However, it is not a cure and should always complement, not replace, medical treatment and advice from your healthcare provider. It helps manage the underlying inflammation.
Q6: What are the main foods I should avoid to reduce inflammation?
A6: To reduce inflammation, I recommend minimizing processed junk foods, sugary drinks and refined sugars, refined carbohydrates (like white bread), trans fats, and excessive red or processed meats. These foods tend to actively promote inflammation within the body, counteracting the benefits of anti-inflammatory foods.
Q7: Can personalized nutrition really help with my inflammation?
A7: Emerging research suggests personalized nutrition, which considers your unique genetics and gut microbiome, can offer highly effective strategies to manage inflammation. This approach helps identify the most beneficial anti-inflammatory foods and dietary patterns specifically for you, moving beyond one-size-fits-all recommendations.
For more information, visit: Anti-Inflammatory Food Benefits












Post Comment