Understanding Eye Pain: What Your Eyes Are Telling You
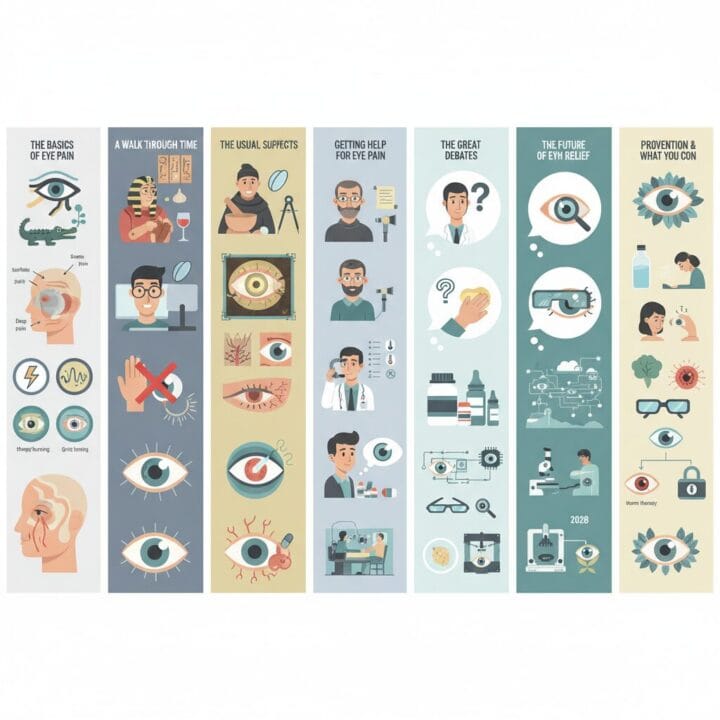
Table of Contents
Understanding Eye Pain: What Your Eyes Are Telling You
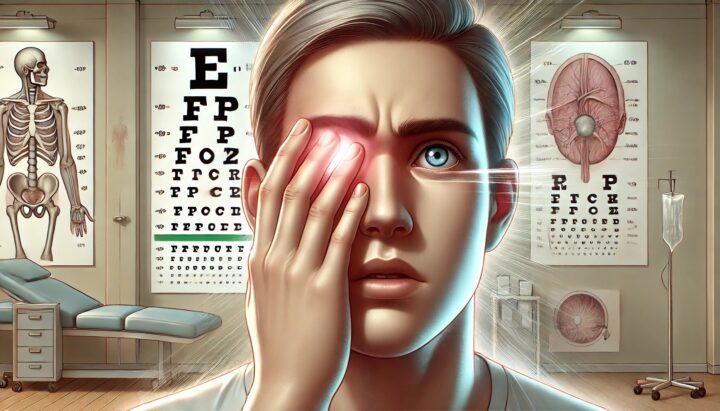
We’ve all been there: a sudden, unwelcome sensation in our eye, ranging from a mild irritation to a sharp, throbbing ache. Eye pain, medically known as ophthalmalgia, is more than just a nuisance; it’s our body’s way of signaling that something isn’t quite right. Whether it feels like a persistent grit, a burning sensation, or a deep pressure behind your eye, understanding these different signals can be the first step toward finding relief and preserving your vision.
Eye pain can broadly be categorized by where it occurs. Ocular pain refers to discomfort on the surface of the eye. This often feels like itching, burning, or a scratching sensation, and usually points to external irritations, infections, or minor trauma. Think of a tiny eyelash stuck under your lid or the sting of a chemical splash. On the other hand, orbital pain is felt deeper within the eye, often described as an aching, throbbing, or stabbing sensation. This type of pain can indicate a more serious underlying condition, such as inflammation inside the eye or increased pressure. Recognizing this difference helps us know when a simple solution might suffice and when it’s time to seek professional medical advice.
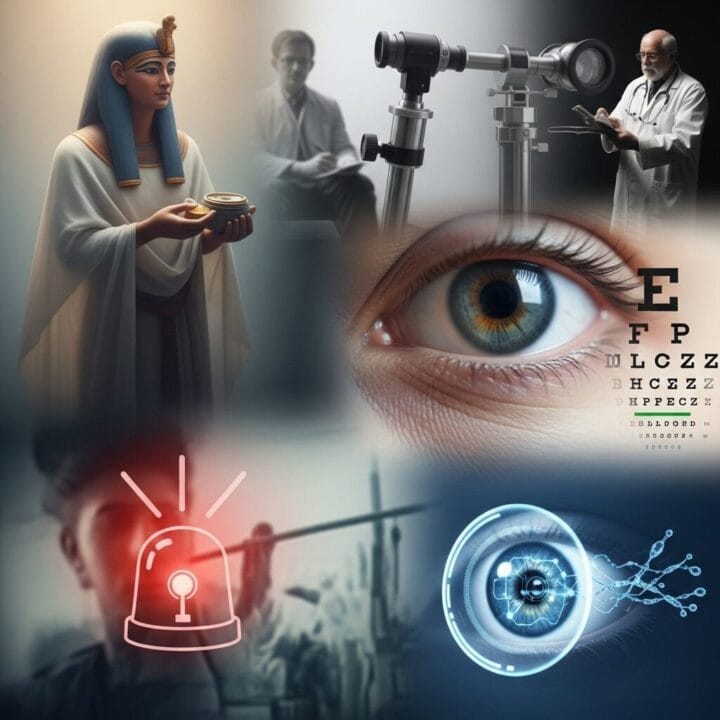
A Journey Through Time: How We’ve Understood and Treated Eye Pain
Our approach to eye pain has evolved dramatically over centuries. In ancient Egypt, as early as 1550 BCE, medical texts like the Ebers Papyrus described remedies for eye conditions using intriguing ingredients such as crocodile dung and various salts. Ancient Indian texts, particularly the Sushruta Samhita (between 1000 and 600 BCE), detailed dozens of eye conditions and surgical methods, with Sushruta himself credited as the first known cataract surgeon. His technique, called “couching,” involved dislodging the clouded lens to clear the visual path, though patients remained without a functional lens. Our ancestors saw the eyes not just as organs of sight but as “windows to the soul,” emphasizing their vital importance and the distress caused by any pain.
Moving into the medieval period, practices continued to blend observation with unique concoctions. Bald’s Leechbook, a 10th-century Anglo-Saxon text, included an eye salve made from garlic, onion or leek, wine, and bovine bile. Remarkably, modern research has shown this ancient remedy to possess strong antibiotic properties, even effective against resistant bacteria like MRSA. This highlights how ancient wisdom, even with its unusual methods, sometimes stumbled upon effective treatments.
The true scientific study of the eye began to solidify in the Renaissance, with significant strides in the 18th and 19th centuries. Georg Bartisch’s Ophthalmodouleia (1583) laid foundational knowledge. The 18th century saw the first planned cataract extraction by Jacques Daviel. Then came German physician Hermann von Helmholtz, who invented the ophthalmoscope in 1851. This device was a game-changer, allowing doctors to look directly inside the eye, revolutionizing diagnosis. Albrecht von Graefe, a “father of modern ophthalmology,” further advanced our understanding of glaucoma and introduced new surgical techniques. From crocodile dung to sophisticated optical instruments, our journey to combat eye pain reflects humanity’s persistent quest to preserve this precious sense.
Common Culprits: What’s Making Your Eyes Hurt Today?
If your eyes are aching, you’re not alone. Many factors can cause eye pain, ranging from minor irritations to more serious conditions that require attention. Let’s explore some of the most common reasons why your eyes might be bothering you.
Everyday Irritants and Digital Strain
Sometimes, the cause of eye pain is straightforward. Have you ever felt like something is in your eye, a gritty, sandy sensation that just won’t go away? That’s often a foreign object – a tiny speck of dust, an eyelash, or a bit of makeup. These minor irritants can cause significant discomfort, especially when you blink. Contact lens mishaps are another frequent offender. Wearing lenses too long, not cleaning them properly, or having ill-fitting ones can lead to irritation and even infections.
In our digital world, screen time is a leading cause of eye strain and discomfort. Staring at computers, phones, and tablets for extended periods can lead to dry eyes, headaches, and a general aching sensation. This happens because we tend to blink less when focusing on screens, and the constant focus can strain our eye muscles.
Infections and Inflammations: The “Pink Eye” Brigade
Eye infections are a common source of pain and discomfort. The most well-known is conjunctivitis, often called “pink eye.” This inflammation of the clear membrane covering the white part of your eye can be caused by viruses, bacteria, or allergies. Viral pink eye often brings burning, redness, and watery eyes, while bacterial forms can cause a sore, red eye with sticky discharge. Allergic conjunctivitis typically results in itchy, red, and watery eyes, sometimes with a gritty feeling.
Beyond pink eye, other infections and inflammations can cause significant pain:
- Blepharitis: This is an inflammation of the eyelids, often caused by clogged oil glands at the base of your eyelashes. It can lead to swollen, itchy eyelids and a burning or sore sensation.
- Styes and Chalazions: A stye is a painful, tender bump on the eyelid, usually caused by an infected eyelash follicle or oil gland. A chalazion is a similar, but typically less painful, lump from a blocked oil gland. Both can make blinking uncomfortable.
- Corneal Abrasions and Ulcers: A corneal abrasion is a scratch on the clear front surface of your eye. These can be very painful but often heal quickly. A more serious condition, a corneal ulcer, is an open sore on the cornea, usually resulting from an infection or injury, and can be severely painful.
- Inflammation Inside the Eye: Conditions like uveitis or iritis involve inflammation of the eye’s internal structures. These can cause pain, redness, light sensitivity, and even reduced vision, often stemming from trauma, infections, or autoimmune issues. Optic neuritis, inflammation of the optic nerve that connects your eye to your brain, can cause deep discomfort, especially with eye movement, and vision loss.
Pressure and Headaches: Glaucoma, Sinus, and Migraines
Sometimes, eye pain originates from increased pressure or is referred from other areas of the head.
- Glaucoma: This condition damages the optic nerve, often due to increased pressure inside the eye. While many types are painless in their early stages, acute angle-closure glaucoma is a medical emergency. It causes a sudden, severe increase in eye pressure, leading to intense eye pain, headache, nausea, vomiting, and vision loss. Recognizing these symptoms and seeking immediate care is vital to prevent permanent damage.
- Sinus Infections (Sinusitis): Our sinuses are hollow, air-filled spaces around our eyes and nose. When they become inflamed or infected, the pressure buildup can cause a dull ache or throbbing pain behind or around your eyes. This pressure can also lead to eyelid swelling and puffiness.
- Headaches: Migraines and cluster headaches often bring eye pain along for the ride. Migraines can cause a severe, throbbing pain, often behind one eye, accompanied by sensitivity to light and sound. Cluster headaches are characterized by intense, sharp pain around one eye, sometimes with a watery eye and drooping eyelid on the affected side.
Understanding these common causes can help you identify potential triggers and know when it’s time to consult an eye care professional.
Seeking Help: When to Consult an Eye Doctor for Your Pain
Not all eye pain requires an emergency room visit, but knowing the “red flags” can make all the difference. While a simple warm compress might resolve a minor irritation, certain symptoms demand immediate professional attention to protect your vision.
When to Seek Immediate Medical Attention
You should seek prompt medical care if your eye pain is accompanied by any of these urgent symptoms:
- Sudden, severe eye pain that comes on intensely.
- Any loss of vision or sudden changes in your sight, such as blurred vision, dark spots, seeing halos around lights, or flashes of light.
- Severe headache, especially if it’s new or the “worst headache of your life.”
- Nausea or vomiting alongside eye pain.
- Neck stiffness with light sensitivity.
- Confusion or disorientation.
- Evidence of trauma to the eye or head, such as a direct blow or a chemical splash.
- Trouble moving your eye normally or inability to keep it open.
- Blood or pus coming from your eyes.
- Significant swelling or redness in or around your eyes.
- Fever or chills, indicating a possible body-wide infection.
- Pain after recent eye surgery or injection.
If you experience any of these, call an eye care professional or go to an emergency room right away. Timely diagnosis and treatment are crucial to prevent permanent damage.
What to Expect at the Eye Doctor’s Office
When you visit an eye doctor for pain, they will conduct a thorough examination. This usually involves:
- A vision check: To assess any changes in your visual acuity.
- External examination: Looking for redness, swelling, or foreign bodies on your eyelids and the surface of your eye.
- Slit lamp examination: Using a specialized microscope with a bright light to get a magnified view of your eye’s front structures, including the cornea, iris, and lens. This helps detect abrasions, infections, or inflammation.
- Fluorescein staining: A dye may be applied to your eye to highlight any scratches or ulcers on the cornea when viewed under a blue light.
- Eye pressure check (tonometry): Measuring the pressure inside your eyes to rule out conditions like glaucoma.
- Dilated exam: Eye drops might be used to enlarge your pupils, allowing the doctor to examine the retina and optic nerve at the back of your eye.
First Aid and Treatment Options
For milder forms of eye pain, some simple steps can offer relief:
- Warm compresses: For conditions like styes or blepharitis, a warm, clean washcloth placed on closed eyelids for a few minutes can help soothe the area and loosen clogged glands.
- Saline rinses or artificial tears: If you suspect a foreign object, gently flushing your eye with clean water or saline solution can help. Artificial tears can lubricate dry eyes and reduce irritation.
- Rest: Giving your eyes a break, especially from digital screens, can often alleviate pain caused by eye strain.
- Over-the-counter pain relievers: Medications like ibuprofen can help manage general discomfort.
When a diagnosis is made, your doctor will recommend a targeted treatment plan:
- Eye drops: Depending on the cause, these could be antibiotics for infections, antihistamines for allergies, corticosteroids for inflammation, or special drops to reduce eye pressure for glaucoma.
- Oral medications: Sometimes, oral antibiotics, anti-inflammatory drugs, or pain relievers are prescribed.
- Corrective lenses: If your pain is due to uncorrected vision problems or eye strain, new glasses or contact lenses, possibly with anti-glare or blue light filters, might be recommended.
- Surgery: In severe cases, such as certain types of glaucoma, significant trauma, or infections that don’t respond to other treatments, surgery may be necessary.
It’s important to follow your doctor’s advice and not attempt to remove embedded foreign objects or treat severe eye pain on your own.
Unanswered Questions and Future Directions in Eye Pain Management
Even with our advanced medical knowledge, eye pain can present complex challenges. One such mystery is “pain without stain,” known as neuropathic ocular pain (NOP). These patients experience significant eye pain, often a burning or gritty sensation, but their eyes appear normal upon examination, with no obvious signs of inflammation or damage. This condition points to problems with the corneal nerves or central nervous system, making it a real head-scratcher for doctors. Diagnosing NOP is primarily clinical, meaning it relies on a patient’s symptoms rather than physical signs, and treatments often draw from approaches used for other chronic nerve pain conditions, as specific ophthalmic data are still emerging.
Another ongoing discussion involves the initial management of acute eye problems. Many patients first visit general practitioners or emergency departments, where topical antibiotic therapy is often overprescribed for conditions that might be viral or allergic. Experts emphasize that symptoms like pain, light sensitivity, or blurred vision with a red eye almost always signal a serious condition that requires immediate referral to an ophthalmologist, rather than just an antibiotic prescription. The challenge lies in primary care settings often lacking the specialized equipment, like a slit lamp microscope, needed to accurately diagnose conditions such as iritis or acute glaucoma.
Tomorrow’s Solutions: Promising Innovations for Eye Pain Relief
The future of eye pain relief looks promising, with ongoing research and emerging technologies focused on more targeted and effective treatments.
- Targeting Nerve Pain: New drugs are in development, like topical ocular OK-101, designed to alleviate severe pain from corneal nerve damage. This non-opioid candidate aims to stay on the eye surface longer to provide sustained relief. Beyond drops, therapies using nerve blocks or stimulation, such as trigeminal nerve stimulation, are showing effectiveness in reducing chronic ocular pain, including sensitivity to light and wind.
- Cooling Devices: Imagine a device that gently cools your eyes for a few minutes to provide instant relief. EyeCool Therapeutics is developing such a device, ETX-4143, which has shown positive pilot study results for chronic ocular surface pain by targeting specific nerves.
- Regenerative Medicine: This exciting field explores how we might repair damaged eye tissues. Stem cell therapy holds the promise of regenerating corneal tissue or protecting the optic nerve, potentially decreasing pain and slowing vision loss. Researchers are even working on 3D bioprinting customized artificial corneas, offering a renewable source for transplantation and reducing rejection risks.
- Smart Technology: The future could bring smart contact lenses that monitor your eye pressure or detect early signs of dry eye. Artificial intelligence (AI) is increasingly being used to analyze retinal scans for early disease detection and to personalize treatment plans, moving towards more predictive and preventative care. Neurolens technology is already tackling digital eye strain and misalignment, using micro prism technology to correct vision and reduce muscle strain.
- Gene Therapy: Breakthroughs in gene therapy, such as recent research allowing retinal cells to produce antibodies that block proteins hindering eye healing, could revolutionize treatment for conditions like macular degeneration and diabetic retinopathy. Human trials are even slated for 2028.
- Next-Generation Eye Drops: The pipeline for new eye drops is robust, with medications like Reproxalap, OCS-02, and Tryptyr (acoltremon) offering fresh hope for dry eye disease and inflammation by stimulating natural tear production or reducing discomfort.
These innovations are moving us towards a future where eye pain is not only better understood but also more effectively treated, offering improved quality of life for millions.
Keeping Your Eyes Healthy: Prevention and Self-Care Tips
Protecting your eyes is often about adopting simple, consistent habits. While we can’t prevent every issue, many common causes of eye pain are manageable through mindful care.
- Practice Good Eye Hygiene: Wash your hands frequently, especially before touching your eyes or handling contact lenses. Always remove makeup thoroughly before bed to prevent irritation and infections.
- Contact Lens Care: If you wear contact lenses, follow your eye doctor’s instructions carefully. This means cleaning them properly, replacing them on schedule, and never sleeping in them unless specifically approved by your doctor. If you experience pain while wearing contacts, remove them immediately and consult your eye care professional.
- Reduce Digital Eye Strain: Take regular breaks using the 20-20-20 rule: every 20 minutes, look at something 20 feet away for 20 seconds. Ensure your screen is positioned correctly, and consider using anti-glare filters or blue light blocking glasses.
- Protect Your Eyes: Wear appropriate protective eyewear during sports, yard work, or when exposed to chemicals or airborne particles. Wraparound sunglasses can shield your eyes from wind, dust, and harmful UV rays, which can contribute to dryness and irritation.
- Stay Hydrated and Nourished: Drink plenty of water throughout the day to support overall body hydration, including tear production. A diet rich in Omega-3 fatty acids (found in fish, flaxseed, walnuts) can also promote healthy oil glands in your eyes.
- Know When to Act: For minor irritation, a warm compress or artificial tears might be all you need. However, if your eye pain is severe, persistent, accompanied by vision changes, light sensitivity, or other concerning symptoms like fever or nausea, it’s always best to consult an eye care professional without delay. They can accurately diagnose the cause and recommend the most appropriate treatment, ensuring your precious vision is protected.
Remember, your eyes are vital, and paying attention to their signals is key to maintaining good eye health. Don’t hesitate to seek professional advice when pain or discomfort goes beyond simple, temporary irritation.












Post Comment