Understanding Tension Type Headache: Your Guide to Relief
Table of Contents
Understanding Tension Type Headache: Your Guide to Relief
Have you ever felt like your head is caught in a vise, a persistent squeeze that just won’t let go? If so, you’re likely familiar with a tension type headache. This common condition affects millions of us, bringing a dull, constant ache or pressure across the forehead, sides, or back of the head. Unlike the throbbing sensation of a migraine, a tension type headache usually feels like a steady pressure and typically doesn’t worsen with everyday activities like walking. Many people also notice tenderness in their neck and shoulders, and sometimes, especially with chronic forms, a slight sensitivity to light or sound can accompany the pain. We see these headaches appear in different ways: infrequently, a few times a month, or, for some, far too often, becoming a part of daily life. Understanding this common headache and its nuances is the first step toward finding lasting relief.
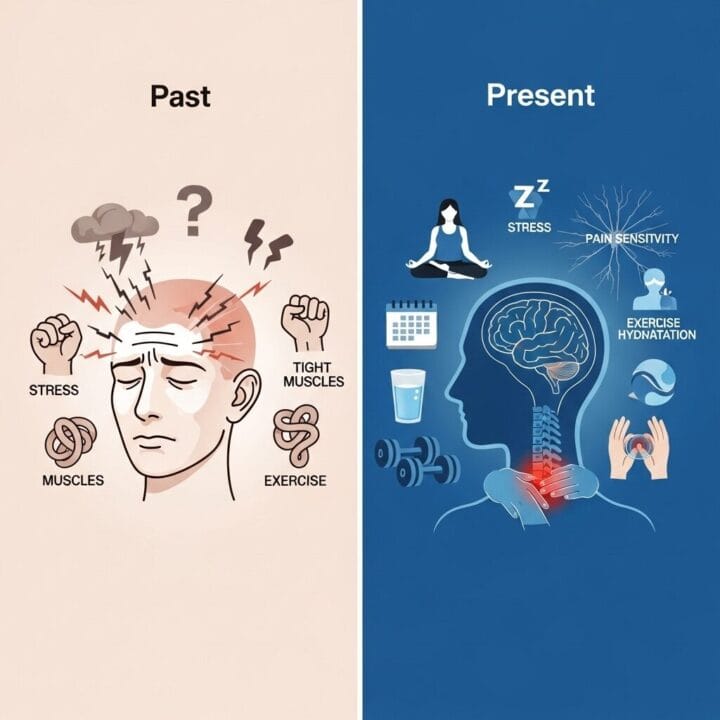
The Evolving View of Headaches: From Simple Stress to Complex Pain
Our understanding of headaches, particularly the tension type headache, has come a long way. Believe it or not, doctors haven’t always viewed these headaches the way we do today. In the 1950s, medical professionals began the important work of distinguishing various headache types, trying to separate what we now know as tension headaches from migraines.
Early Ideas about Headache Causes
- “In Your Head” Origin: For a long time, many believed that headaches like these were primarily psychological, stemming purely from mental tension or emotional distress.
- Muscle Contraction Focus: Another dominant theory was the “muscle contraction headache” or “stress headache.” The idea was that overly tight muscles in the head, neck, and shoulders were the sole culprits.
However, medical insights evolved. By 1988, the International Headache Society introduced a more comprehensive headache classification system. This new system officially recognized the tension type headache as a distinct condition, moving beyond the idea that it was only about muscle contraction. Researchers started considering the role of pain sensitivity, acknowledging that the underlying mechanisms were more complex than previously thought. This shift marked a significant turning point, even if tension type headaches still receive less research attention compared to migraines. This ongoing journey of discovery highlights how dynamic medical knowledge can be, constantly adapting as we learn more about the human body.
The “Why Me?” Question: What Really Causes Tension Type Headache Pressure?
It’s natural to wonder why you get these persistent head pressures. The truth is, no one is 100% certain of the exact cause, but current medical understanding offers some solid clues that go beyond just tight muscles.
Common Triggers We All Experience
We know that many everyday factors can set off a tension type headache:
- Stress: Emotional or mental strain is a leading trigger. Think about those days filled with deadlines or personal worries.
- Poor Sleep: Not getting enough restful sleep or experiencing inconsistent sleep patterns often contributes.
- Dehydration: Simply not drinking enough water can be a surprising but potent trigger.
- Hunger: Skipping meals can also lead to a headache.
- Caffeine Habits: Both excessive caffeine intake and withdrawal from caffeine can trigger symptoms.
- Poor Posture: Hunching over a computer or phone for extended periods puts strain on your neck and shoulders, a common cause of tension headaches.
- Eye Strain: Hours spent staring at screens without breaks can also contribute.
But the latest thinking in medicine suggests something more profound. While those muscles in your neck and shoulders might indeed feel tight, they are often a symptom, not the whole story. Many researchers now believe that a tension type headache is more about your body’s pain system becoming extra sensitive. It’s a complex interplay involving genetic predispositions, environmental factors, and how your brain processes pain signals. For instance, some individuals might have a naturally lower pain threshold, making them more susceptible. It’s not just a physical squeeze; it’s a subtle recalibration of how your brain experiences discomfort.
My friend, Sarah, used to get these headaches almost daily after long hours at her desk. “I thought it was just bad posture,” she told me, “but even when I tried to sit up straight, they came back. It wasn’t until I started managing my stress and prioritizing sleep that I really saw a difference. It’s like my whole system was on high alert.” Sarah’s experience shows how connected our physical and mental states are when it comes to headaches.
Getting the Right Label: Is It Just a Tension Headache or Something More?
Pinpointing the exact type of headache you’re experiencing is crucial for effective treatment. When you talk to your doctor about a tension type headache, they usually rely on a thorough conversation about your symptoms and a physical check-up. We don’t typically need fancy scans unless there are unusual or concerning signs.
Key Diagnostic Signs for Tension Type Headache
Doctors use specific criteria to diagnose a tension type headache, often based on guidelines from organizations like the International Headache Society:
- Bilateral Pain: The pain usually affects both sides of your head.
- Pressing or Tightening Quality: It feels more like pressure or a tight band, rather than a throbbing sensation.
- Mild-to-Moderate Intensity: The pain is usually not severe enough to stop you from daily activities.
- Not Worsened by Activity: Unlike migraines, routine physical activity generally does not intensify the headache.
- Absence of Severe Migraine-Like Symptoms: Typically, there’s no severe nausea, vomiting, or extreme sensitivity to light or sound.

The Gray Area: Overlapping Symptoms
This is where things can get a bit tricky. Sometimes, it’s not a clear-cut distinction between a tension type headache and a milder migraine. Their symptoms can overlap, making diagnosis challenging. For example, with a chronic tension headache, you might occasionally experience mild nausea or a slight sensitivity to light or sound. This overlap can sometimes lead to an initial misdiagnosis. I once had a client who spent years treating what she thought were migraines, only to find out with a specialist that her persistent head pressure and mild light sensitivity were actually symptoms of a severe chronic tension headache exacerbated by jaw clenching. Her treatment plan shifted dramatically once the correct diagnosis was made. Therefore, describing all your symptoms accurately to your doctor, even the subtle ones, is incredibly important.
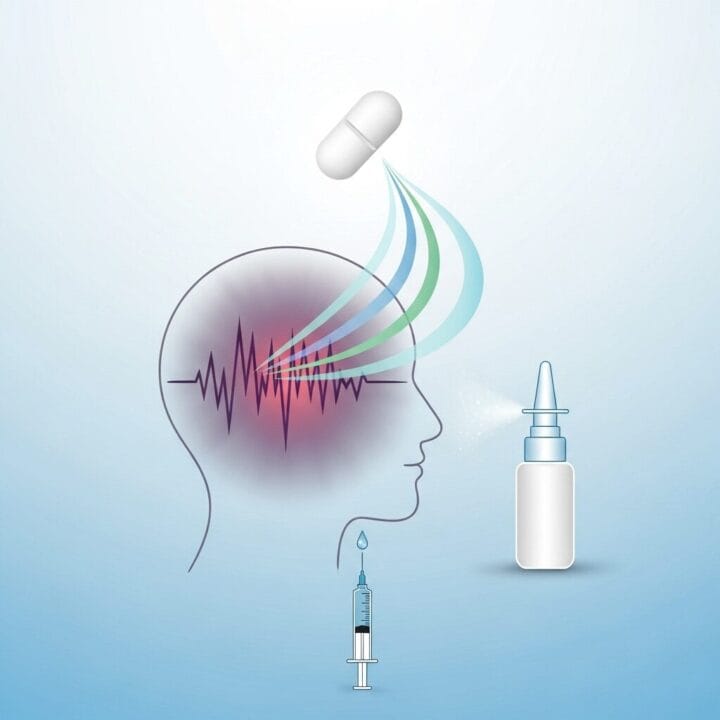
Finding Your Zen: How to Tackle Tension Type Headaches Today
When you’re dealing with a tension type headache, finding effective ways to manage the pain and prevent future episodes is key. We often categorize relief strategies into quick fixes for immediate comfort and long-term approaches for sustained well-being.
Quick Fixes (Use with Caution!)
For immediate relief from a mild to moderate tension type headache, many people turn to over-the-counter pain medications. These might include:
- Ibuprofen: A nonsteroidal anti-inflammatory drug (NSAID).
- Acetaminophen: A common pain reliever.
- Aspirin: Another NSAID that can help with pain and inflammation.
Some formulations even combine these with caffeine for an extra boost in relief. However, I must give you a critical warning: do not overuse acute pain medications! Taking them more than two days a week can ironically lead to more headaches. This phenomenon is known as medication-overuse headache, or “rebound headache,” where the medication itself starts causing the pain.
Long-Term Strategy (Prevention is Your Best Friend!)
True lasting relief often comes from a comprehensive prevention plan. This can involve a mix of medical treatments and lifestyle adjustments.
Medication for Prevention
For those with frequent or chronic tension type headaches, doctors might suggest preventive medications.
- Tricyclic Antidepressants: Drugs like amitriptyline are often the first line of defense. They work by affecting brain chemicals to reduce headache frequency and severity.
- Other Medications: Sometimes, other antidepressants, anti-seizure medications, or even muscle relaxants are explored, particularly if initial treatments aren’t fully effective.
Lifestyle Power-Ups: Your Everyday Toolkit
This is where you have significant power. Lifestyle changes are crucial for managing and preventing a tension type headache.
- Stress Management: Since stress is a major trigger, learning to manage it effectively is paramount. Techniques like cognitive behavioral therapy (CBT), biofeedback, mindfulness, and simple relaxation exercises (deep breathing, meditation) can make a huge difference.
- Consistent Sleep: Aim for regular sleep patterns. Going to bed and waking up at the same time each day, even on weekends, can regulate your body’s rhythm.
- Regular Meals and Hydration: Don’t skip meals, and make sure you’re drinking enough water throughout the day. Dehydration and low blood sugar are common headache triggers.
- Regular Exercise: Physical activity releases natural pain-blocking chemicals and can reduce stress.
- Improve Posture: Be mindful of how you sit and stand, especially if you spend a lot of time at a desk or looking at screens. Consider ergonomic adjustments to your workspace.
- Eye Care: Take regular breaks from screens, follow the 20-20-20 rule (every 20 minutes, look at something 20 feet away for 20 seconds), and ensure your eyewear prescription is up to date.
Hands-On Help for Muscle Tension
Many people find relief from therapies that address physical tension:
- Massage Therapy: Gentle massage of your head, neck, and shoulders can help release tight muscles and improve blood flow.
- Physical Therapy: A physical therapist can teach you exercises and stretches to strengthen weak muscles, improve posture, and alleviate muscle imbalances.
- Acupuncture: Some individuals report relief from chronic pain, including tension type headaches, through acupuncture.
- Temperature Therapy: Applying heat (a warm compress, heating pad, or hot shower) or cold (an ice pack or cool washcloth) to tense muscles can provide soothing relief.
Ultimately, finding what works for you often means trying a combination of these approaches. It’s a personalized journey, and what helps one person might be different for another. Don’t hesitate to discuss these options with your doctor to create a tailored plan.
Controversies and the Gray Areas of Tension Type Headache
While tension type headache is incredibly common, it’s also surrounded by ongoing debates and areas of uncertainty, particularly regarding its precise causes and how it relates to other headache types. These controversies highlight the complexity of pain and the challenges in diagnosis and treatment.
Blurring Lines with Migraine
One of the most significant discussions revolves around distinguishing tension type headaches from migraines, especially milder forms. We know they are both primary headaches, meaning they aren’t caused by another underlying condition. However, symptoms can overlap, making diagnosis tricky. For example:
- Shared Triggers: Both can be triggered by stress, lack of sleep, or hormonal changes.
- Mild Sensitivity: While severe light or sound sensitivity is a hallmark of migraine, a chronic tension type headache can sometimes involve mild sensitivity to either.
- Nausea: Though less common, some individuals with chronic tension type headaches may experience mild nausea.
This overlap can lead to diagnostic ambiguity. We might sometimes confuse a less severe migraine for a tension headache, or vice-versa. Doctors rely on patterns – if your headaches are consistently throbbing, one-sided, and accompanied by severe nausea or visual disturbances, it’s more likely a migraine. But for many, the picture isn’t so clear, and a thorough medical history remains the best tool.
The Evolving Understanding of Causes
The very name “tension type headache” suggests stress and muscle tension are the primary drivers. And while they are undeniably factors, the science has moved beyond this singular view:
- Beyond Muscle Contraction: Early theories focused almost exclusively on tightened muscles in the head and neck. However, research now suggests that while muscle tension can aggravate pain, it’s often a symptom rather than the sole root cause. The International Headache Society specifically moved away from terms like “muscle contraction headache” to reflect this updated understanding.
- Pain Sensitivity and Neurobiology: The current prevailing theory emphasizes that individuals with tension type headaches may have an increased sensitivity to pain. This involves complex changes in how the brain and nervous system process pain signals, a concept called central sensitization. This means that for some, the brain becomes “tuned” to perceive even minor stimuli as painful, especially in chronic cases. This neurobiological perspective adds layers of complexity, showing that the issue isn’t just physical tension but also how your brain handles pain.
- Genetic and Environmental Mix: We also understand that both our genes and our environment play a role. Environmental factors like stress might influence episodic headaches more, while genetic predispositions could be more significant in developing chronic tension type headaches.
These ongoing discussions emphasize that understanding and treating tension type headaches requires looking beyond simple explanations and embracing the multifaceted nature of pain.
What’s Next for Tension Type Headache Relief? The Future’s Looking Brighter!
The journey to completely understanding and effectively treating tension type headache is ongoing, but the future holds promise. Researchers are tirelessly working to unlock the remaining mysteries of this pervasive condition, aiming for more precise and personalized solutions.
Cutting-Edge Research Areas
- Central Sensitization: A major focus of current research is “central sensitization” – how your brain and spinal cord become more sensitive to pain signals over time. We believe this mechanism is crucial in why some people develop chronic tension type headaches. Scientists are exploring ways to interrupt or reverse this increased sensitivity.
- Neurotransmitter Roles: Researchers are investigating the role of specific brain chemicals and pathways, such as nitric oxide and calcitonin gene-related peptide (CGRP), in triggering and sustaining tension type headaches. While anti-CGRP medications have seen success in migraine treatment, their effectiveness for tension type headaches is still being evaluated.
- Advanced Imaging and Models: Using advanced tools like brain imaging (fMRI) and developing sophisticated animal models, scientists are getting a clearer picture of what happens in the brain during a tension type headache. These insights are vital for identifying new targets for drug development.
Emerging Treatments and Holistic Approaches
While medications like tricyclic antidepressants remain important for prevention, the field is expanding.
- Targeting Pain Pathways: New compounds that can modify pain sensitivity, such as NMDA-receptor antagonists and nitric oxide synthase inhibitors, are showing early promise. We are excited about the potential for more specific and effective treatments to emerge from this work.
- Personalized Treatment Plans: The future will likely bring an even greater emphasis on personalized care. This means combining the best of medication with tailored behavioral therapies, advanced stress management techniques, and all those healthy habits we’ve discussed. Imagine a treatment plan built specifically for your unique genetic profile, lifestyle, and headache triggers!
- Integrative Medicine: There’s a growing recognition of the power of non-pharmacological and integrative approaches. Therapies focusing on relaxation, stress reduction, and natural pain modulation are gaining more evidence for their effectiveness, offering attractive options for those who prefer to avoid medication or need complementary strategies.
My colleague, Dr. Elena Rodriguez, a neurologist specializing in headache disorders, often remarks, “We’re moving towards a future where managing tension type headaches isn’t just about masking symptoms, but about truly understanding and rebalancing the body’s pain systems. The integration of technology with human-centered care is going to be transformative.”
The goal is clear: to develop better ways to prevent and treat tension type headaches, so fewer people are stuck feeling like their head is in a vise. We are optimistic that continued research will lead to a brighter future for those living with this common pain.
Frequently Asked Questions About Tension Type Headache
Q1: What exactly does a tension type headache feel like?
A tension type headache typically feels like a dull, aching pain or pressure, often described as a tight band squeezing around your forehead, temples, or the back of your head. It’s usually on both sides of the head and not throbbing.
Q2: How is a tension type headache different from a migraine?
A tension type headache is generally milder, non-throbbing, affects both sides, and isn’t usually worsened by physical activity. Migraines often cause moderate to severe throbbing pain, usually on one side, and can be accompanied by severe nausea, vomiting, or extreme sensitivity to light and sound.
Q3: What are common causes of tension type headaches?
Common causes include stress, lack of sleep, dehydration, hunger, eye strain, poor posture, and muscle tension in the neck and shoulders. Current thinking also points to an increased sensitivity of your body’s pain system.
Q4: Can I get a tension type headache every day?
Yes, if headaches occur 15 or more days a month for at least three months, they are classified as chronic tension type headaches. These can significantly impact daily life and often require a long-term management plan.
Q5: What are the best ways to relieve a tension type headache without medication?
Effective non-medication strategies include stress management techniques (like meditation or deep breathing), getting enough consistent sleep, staying well-hydrated, eating regular meals, applying heat or cold packs, and massage for muscle tension.
Q6: When should I see a doctor for my tension type headaches?
You should see a doctor if your headaches are frequent (more than twice a week), severe, disrupt your daily activities, or if you experience any concerning new symptoms like fever, stiff neck, vision changes, or confusion.
Q7: How can I prevent recurring tension type headaches?
Preventive strategies often combine lifestyle changes (stress management, consistent sleep, regular exercise, good posture) with potential preventive medications like tricyclic antidepressants, especially for frequent or chronic tension type headache episodes.
Ready to find lasting relief from your tension type headaches? Take the first step towards a clearer, more comfortable life by consulting a healthcare professional to discuss a personalized management plan.











Post Comment