Understanding Your Daily Headache: Causes, Types, and Relief
Table of Contents
Understanding Your Daily Headache: Causes, Types, and Relief
If you’re experiencing a daily headache, you understand the profound impact persistent pain can have on your life. Many of us have felt that relentless pressure, the throbbing behind the eyes, or the constant ache that never seems to fully disappear. We’re not talking about an occasional head thump here; we’re focusing on Chronic Daily Headaches (CDH), a condition defined by having a headache 15 or more days a month for at least three months. This isn’t a single diagnosis but rather an umbrella term that covers various types of headaches. Imagine a house guest who simply won’t leave, making daily tasks challenging and dimming life’s enjoyment. In this article, we’ll explore what causes these frequent headaches, their different forms, and effective strategies for finding lasting relief. Our goal is to empower you with objective, professional, and actionable information, helping you understand this common yet debilitating condition.
A Headache Through History: From Demons to Brain Storms
For centuries, people have wrestled with persistent head pain, though their understanding and treatments have changed dramatically. In ancient times, for example, our ancestors often believed evil spirits or demons caused headaches. Some even resorted to trepanation, a practice of drilling holes into the skull, possibly to release these perceived malevolent forces. Imagine the bravery, or desperation, required for such a procedure!
Moving to ancient Egypt around 1200 BC, we find references to migraines and nerve-related head pain. Remedies included clay crocodiles bound to the head with linen inscribed with deities’ names, perhaps providing relief through simple pressure. Later, the great Greek physician Hippocrates, around 400 BC, observed that strange visual phenomena often preceded severe head pain. He also linked headaches to stomach troubles, suggesting vapors rising from the gut could be a cause. Roman doctors, influenced by these ideas, incorporated spa treatments and theories about balancing bodily fluids, or “humors,” to alleviate suffering.
Centuries passed, and by the 17th century, Thomas Willis, a pioneer in clinical neuroscience, proposed that headaches were a result of dilated blood vessels. This “vascular theory” gained traction, yet others, like Edward Liveing and William Gowers in the late 1800s, argued for a “neurogenic” theory, suggesting that migraines were brain dysfunctions, like internal “nerve storms.” It wasn’t until the 20th century that scientists began to uncover the complex role of brain chemicals like serotonin, leading to the development of targeted medications, such as triptans, which revolutionized migraine treatment. What a journey from spirits and crocodile remedies to precise neurological insights!
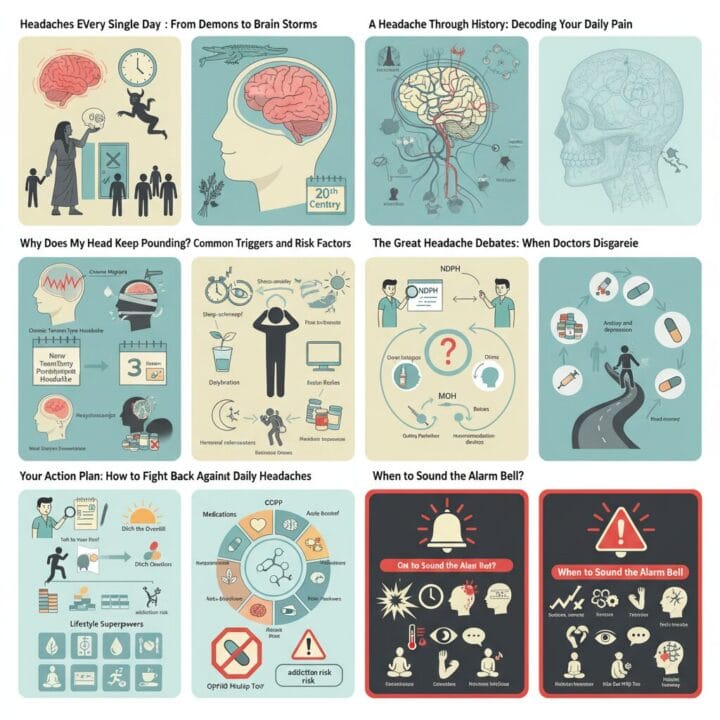
Decoding Your Daily Pain: Understanding Chronic Daily Headache Types
When we talk about a daily headache, it’s important to recognize that this isn’t a single condition but a description for several types of primary and secondary headaches that occur frequently. Understanding which type you experience is the first step toward effective management.
Let’s look at the usual suspects, often called primary headaches, meaning they are not caused by another underlying health problem:
- Chronic Migraine: If you have a history of episodic migraines, they might evolve into chronic migraine, meaning you experience migraine features on 8 or more days per month, and headaches on 15 or more days monthly, for over three months. This often includes throbbing pain, sensitivity to light, sound, or smell, and sometimes nausea or vomiting.
- Chronic Tension-Type Headache: This type usually feels like a constant, dull pressure or a tight band around both sides of your head. The pain is typically mild to moderate and less severe than a migraine, without the strong sensitivity to light or sound.
- New Daily Persistent Headache (NDPH): This is a unique type that begins suddenly, often with a clear start date, and persists daily for three months or longer. The pain can feel like a tension headache or a migraine. What makes it distinct is that it appears without warning and then simply doesn’t go away.
- Hemicrania Continua: This is a rare, continuous headache that affects only one side of your head. It has no pain-free periods and typically causes moderate pain with occasional severe spikes. A key diagnostic feature is its response to a specific anti-inflammatory medication called indomethacin.
- Medication Overuse Headache (MOH): This is a critical one. Sometimes, the very medications you take to relieve headaches, even over-the-counter options, can paradoxically cause more frequent headaches if used too often. This creates a cycle where your head constantly hurts, prompting you to take more medication, which then exacerbates the problem. We refer to this as a “rebound headache.”
Beyond these primary types, sometimes a daily headache can be a secondary headache, a symptom of an underlying health issue. These are less common but require immediate medical attention. Examples include headaches caused by infections, blood vessel problems, brain tumors, or even a past head injury. This is why a thorough medical evaluation is so important.
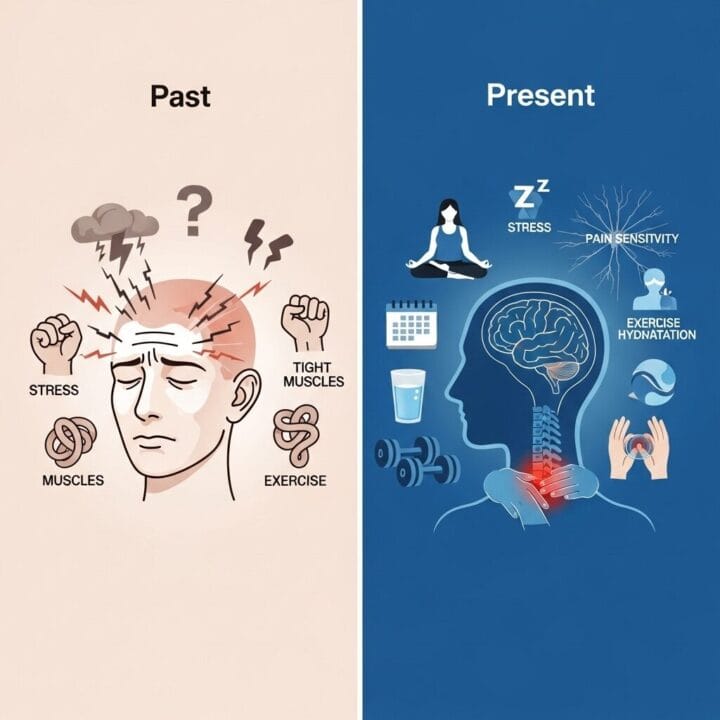
Why Does My Head Keep Pounding? Common Triggers and Risk Factors
Understanding the causes of your frequent head pain is crucial for effective management. While the exact origins of many chronic daily headaches aren’t fully understood, we’ve identified several common triggers and risk factors that can contribute to this relentless discomfort.
Consider these factors:
- Stress and Anxiety: Modern life often brings a constant stream of worries, and our bodies often manifest this mental strain as physical tension. Is it any surprise that stress and anxiety are among the top culprits for frequent headaches? They can tighten muscles in the head and neck, setting the stage for pain.
- Sleep Disturbances: Your sleep pattern plays a significant role. Both too little sleep and, paradoxically, too much sleep can disrupt your body’s natural rhythms and trigger headaches. Are you getting consistent, restful sleep?
- Dehydration and Skipped Meals: Our brains need a steady supply of water and nutrients. Becoming dehydrated or skipping meals can lead to low blood sugar, both of which are common headache triggers. Have you had enough water today?
- Caffeine Overuse or Withdrawal: Many of us rely on caffeine to get through the day. While a small amount can sometimes help, too much caffeine can actually cause headaches, and even withdrawing from it can lead to a headache. It’s a delicate balance.
- Hormonal Changes: For women, fluctuations in hormones, particularly estrogen, can be a major trigger. This often occurs around menstrual cycles, pregnancy, or menopause.
- Poor Posture and Screen Time: Spending hours hunched over a computer or phone can strain your neck and shoulder muscles, leading to tension that radiates into your head. Are you mindful of your posture during the day?
- Medication Overuse: As mentioned, frequently taking acute pain relievers—more than two or three days a week—can lead to medication overuse headaches (MOH). This is a tricky cycle where the medicine intended to help actually perpetuates the pain. This is one of the most common reasons why headaches become a daily occurrence.
- Coexisting Conditions: Conditions like anxiety, depression, obesity, and even snoring can increase your risk of experiencing daily headaches. Addressing these related health issues can sometimes alleviate headache frequency.
Identifying your personal triggers is a powerful step. Keeping a headache diary to track potential culprits can provide valuable insights for you and your healthcare provider.
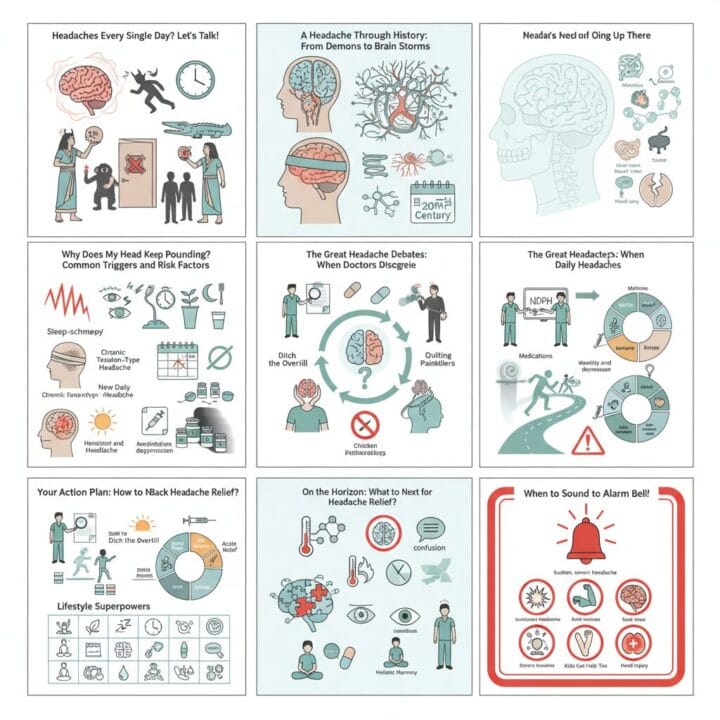
The Great Headache Debates: When Doctors Disagree
Even among medical professionals, there are ongoing discussions and different perspectives regarding the diagnosis and optimal treatment of chronic daily headaches. These debates highlight the complexity of these conditions and the challenges in finding universal solutions.
One area of debate centers on New Daily Persistent Headache (NDPH). While NDPH is characterized by a sudden onset that the patient often remembers clearly, doctors sometimes bicker over its precise classification. Should it primarily include migraine-like symptoms, or is its sudden, unremitting nature the defining characteristic, regardless of other symptoms? Some experts wonder if NDPH is a truly distinct condition or simply a descriptive “bucket term” for a persistent daily headache without a clear cause. This ongoing discussion can affect how NDPH is diagnosed and what treatments are prioritized, as there are no definitive diagnostic tests for it, and its pathophysiology remains poorly understood.
Another significant area of contention involves Medication Overuse Headache (MOH). Here, the “chicken or the egg” dilemma often arises: Is it that taking too many painkillers directly causes the headaches, or are individuals taking more medication because their headaches were already out of control and simply weren’t responding to treatment? While evidence strongly supports that medication overuse is a significant risk factor for chronic headaches, the perceived “blame” on the patient for taking too much medication can be a sensitive issue. Understanding this cycle is crucial, as the primary treatment for MOH involves gradually reducing or stopping the overused medication.
And speaking of medication, the role of opioids in headache treatment is a heated topic. Most headache specialists agree that opioids are generally not a good idea for chronic headaches. Why? Because they carry significant risks of addiction and can actually worsen headaches in the long run, contributing to the very cycle of daily pain we are trying to break. Despite this consensus, these debates continue, emphasizing the need for personalized approaches and continuous research in headache management.
If you suspect you have MOH, consulting your doctor to safely discontinue these medications is essential. This process, often called “detoxification,” can be challenging due to temporary worsening of headaches and other withdrawal symptoms like nausea or anxiety. There’s no single perfect “bridge therapy” to ease this transition, adding another layer to the debate about the most effective withdrawal strategies.
Your Action Plan: How to Fight Back Against Daily Headaches
Living with a daily headache can feel overwhelming, but you have options to reclaim your life. Effective management often involves a partnership with your healthcare provider and a commitment to lifestyle changes.
1. First Things First: Talk to Your Doctor!
Your primary care doctor is your first and most important ally. They will perform a thorough medical history, a physical exam, and potentially recommend blood tests or imaging scans (like an MRI or CT scan) if they suspect a serious underlying cause, known as a “secondary headache.” This detective work is crucial for an accurate diagnosis. A headache diary is your secret weapon here: tracking your headache days, severity, symptoms, and any potential triggers (foods, stress, sleep patterns) provides invaluable information.
2. Ditch the Overkill (for Medication Overuse Headaches):
If your doctor determines you have medication overuse headaches (MOH), the most critical step is to reduce or stop the frequent use of acute pain relievers. This process needs to be carefully managed by your doctor, as withdrawal can temporarily worsen headaches and cause other uncomfortable symptoms. It might be a bumpy road, but it’s essential for breaking the cycle of daily pain and allowing other preventive treatments to work effectively. Your doctor might recommend a “bridge therapy” using a different medication or a short course of steroids to ease this transition.
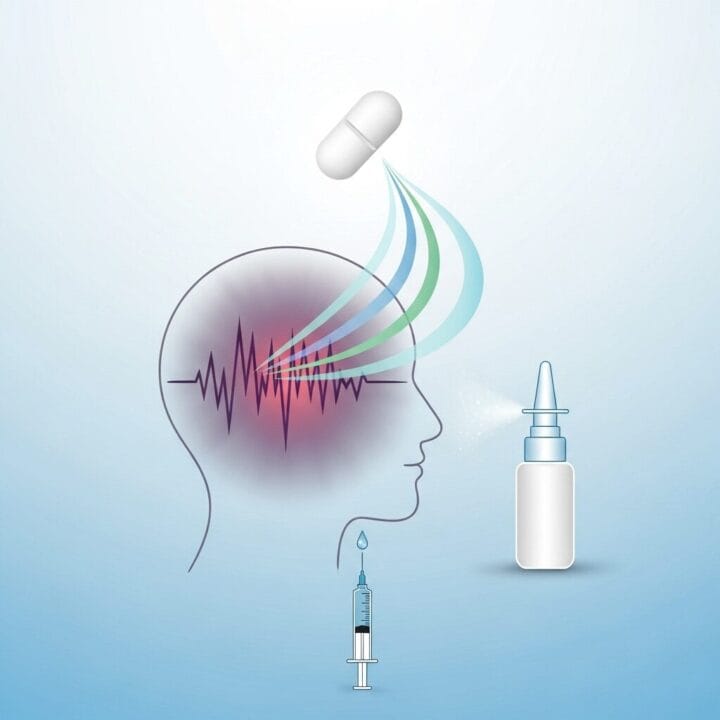
3. Medications That Actually Help (Preventive & Acute):
Once underlying issues are ruled out and medication overuse is addressed, your doctor might suggest specific medications. These fall into two main categories:
- Preventive Medications: Taken regularly, these aim to reduce the frequency and severity of your headaches.
- Antidepressants: Often, low doses of tricyclic antidepressants (like amitriptyline or nortriptyline) are prescribed. They can help with headaches, and also address co-occurring anxiety, depression, and sleep disturbances.
- Beta-blockers: Commonly used for blood pressure, medications like propranolol or metoprolol can also prevent migraines.
- Anti-seizure Medications: Drugs such as topiramate or divalproex sodium may be effective in reducing chronic daily headache frequency.
- Botox Injections: For chronic migraines, injections of Botulinum toxin (Botox) into specific areas of the head and neck every 12 weeks can be a highly effective preventive option.
- CGRP Targeted Therapies: Newer medications (CGRP monoclonal antibodies and oral gepants) specifically target a protein involved in migraine pathways. These can be game-changers for many, offering relief with potentially fewer side effects.
- Acute Relief Medications: These are taken at the first sign of a headache to stop it from becoming severe.
- Triptans: For migraines, drugs like sumatriptan are often prescribed. Use these wisely and only as directed to avoid MOH.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Over-the-counter NSAIDs like ibuprofen or naproxen can relieve tension headaches, but again, be careful not to overuse them.
- Ditans and Oral Gepants: Newer acute treatments like lasmiditan (a ditan) and ubrogepant/rimegepant (oral gepants) are available, often without the vasoconstrictive effects of triptans, making them safer for some individuals.
4. Lifestyle Superpowers: Empower Yourself Daily
Beyond medication, lifestyle adjustments are incredibly powerful in managing daily headache. These are habits you can cultivate to support your overall well-being:
- Chill Out: Stress management techniques are huge. Explore meditation, deep breathing exercises, yoga, or cognitive behavioral therapy (CBT). Learning to calm your nervous system can significantly reduce tension-related headaches.
- Move Your Body: Regular physical activity is a game-changer. Aim for consistent, moderate exercise, like brisk walking, to ease stress and release natural pain-blocking endorphins.
- Sleep Right: Stick to a consistent sleep schedule. Go to bed and wake up around the same time each day, even on weekends. Aim for 7-9 hours of quality sleep.
- Eat Smart: Stay well-hydrated by drinking plenty of water throughout the day. Eat regular meals to avoid blood sugar dips. Identify and avoid any specific food triggers that seem to bring on your headaches.
- Caffeine Check: If you rely heavily on caffeine, consider gradually reducing your intake. A little might help, but too much can fuel your headaches.
- Posture Patrol: Be mindful of your posture, especially if you spend a lot of time at a desk or on screens. Good ergonomics can prevent muscle tension in your neck and shoulders.
Ready to take control of your daily headache? Contact your doctor today to discuss a personalized plan and start your journey toward consistent relief.
On the Horizon: What’s Next for Headache Relief?
The field of headache medicine is constantly evolving, bringing exciting new developments and promising research for those who suffer from daily headache. The future of relief is looking brighter, moving towards more targeted and personalized approaches.
One of the biggest breakthroughs has been in CGRP-targeted therapies. CGRP (calcitonin gene-related peptide) is a protein that plays a key role in transmitting pain signals in the brain during a migraine. Scientists have developed medications that either block the CGRP receptor or target the CGRP molecule itself. These include:
- CGRP Monoclonal Antibodies (mAbs): These are preventive treatments, often given as self-injections monthly or quarterly, or as quarterly intravenous infusions. Medications like erenumab, fremanezumab, galcanezumab, and eptinezumab have offered significant relief for many people with chronic migraine, often with fewer side effects than older preventives.
- Gepants (Oral CGRP Antagonists): These are oral medications that block the CGRP pathway. Ubrogepant and rimegepant are used for acute migraine attacks, while atogepant is approved for migraine prevention. Rimegepant can even be used for both. A newer option, zavegepant, is available as a nasal spray for rapid acute relief. These oral options are particularly valuable as they don’t carry the same risk of medication overuse headaches as some traditional acute treatments and can be safer for individuals with cardiovascular concerns.
Beyond CGRP, researchers are exploring other avenues:
- Ditans: Medications like lasmiditan work differently than triptans, targeting specific serotonin receptors to stop migraine pain without constricting blood vessels, potentially making them safer for some patients.
- Gadget Power (Neuromodulation): This is a fascinating area involving devices that use electrical or magnetic stimulation to influence nerve activity. Non-invasive devices, applied to the forehead or arm, are showing promise in reducing headache frequency and intensity. There’s also research into implanted devices for more severe, refractory cases.
- Beyond CGRP: New Targets: Scientists are looking at other brain chemicals, such as PACAP (pituitary adenylate cyclase-activating polypeptide), to identify new pathways that could be targeted for future treatments. This means more options are likely on the horizon if current therapies aren’t the right fit.
- Personalized Treatment: The future aims to be highly individualized. Instead of a one-size-fits-all approach, healthcare providers will increasingly use patient data and genetic insights to tailor treatment plans precisely to your unique headache profile. This could mean more effective prevention and fewer side effects.
- Holistic Approaches Gain Ground: Non-drug therapies like Cognitive Behavioral Therapy (CBT), mindfulness, and biofeedback continue to be refined and integrated into treatment plans, acknowledging the complex interplay between mind and body in headache conditions. Researchers are also exploring the link between jaw alignment, airway function, and temporomandibular joint (TMJ) disorders to provide long-term relief for some patients.
- Kids Get Help Too: Ongoing research is dedicated to finding FDA-approved migraine prevention medicines specifically for children and adolescents, filling a critical gap in care for younger sufferers of chronic daily headaches.
These advancements signify a shift towards a deeper understanding of headache mechanisms, leading to more effective and safer strategies for managing and preventing frequent headaches. We are moving closer to a future where persistent head pain becomes a manageable, rather than debilitating, condition for more individuals.
When to Sound the Alarm Bell
While many daily headache types are primary and not immediately life-threatening, it’s crucial to know when to seek professional medical attention.
You should definitely see a doctor if:
- Your headaches are daily, getting worse, changing in character, or significantly interfering with your daily life.
- You find yourself relying on over-the-counter pain relievers most days of the week, as this could indicate medication overuse headache.
- Your headache pattern is new and unexplained, especially if you’re over 50.
Seek IMMEDIATE medical help or go to the emergency room if your headache is accompanied by any of these urgent warning signs:
- A sudden, extremely severe headache, often described as the “worst headache of your life” (sometimes called a “thunderclap headache”).
- Headache accompanied by fever, a stiff neck, confusion, vision changes (like blurred or double vision), weakness, numbness, difficulty speaking, or seizures.
- A headache that develops after a head injury.
- A headache that wakes you up from sleep or is consistently present upon waking in the morning, particularly in children.
- Headaches that worsen with coughing, sneezing, or bending over.
- Headaches in someone with a history of cancer or a weakened immune system.
These symptoms could indicate a more serious underlying condition that requires prompt diagnosis and treatment. Always err on the side of caution when your body sends such strong signals.
Frequently Asked Questions About Daily Headaches
Q1: What exactly defines a chronic daily headache?
A chronic daily headache is typically defined as experiencing headaches 15 or more days per month for a period of at least three consecutive months. It’s a descriptive term encompassing several types, not a single diagnosis.
Q2: Can stress really cause a daily headache?
Yes, stress is a very common trigger for daily headaches, particularly chronic tension-type headaches. Prolonged stress can lead to muscle tension in the head and neck, contributing to persistent pain. Learning stress management techniques can be very helpful for daily headache relief.
Q3: What is a medication overuse headache (MOH) and how does it relate to daily headaches?
A medication overuse headache (MOH), also known as a rebound headache, develops when you frequently use acute pain relievers (even over-the-counter ones) more than two or three days a week. This overuse paradoxically causes more frequent and sometimes more severe headaches, leading to a vicious cycle of persistent daily headache.
Q4: Are there new treatments available for chronic migraines, a type of daily headache?
Yes, significant advancements have been made. Newer treatments include CGRP-targeted therapies (monoclonal antibodies and oral gepants) and ditans, which are designed to prevent or acutely treat migraines with different mechanisms than older drugs. Neuromodulation devices are also emerging as promising options for daily headache management.
Q5: When should I see a specialist for my daily headaches?
You should consider seeing a headache specialist or neurologist if your daily headache persists despite primary care efforts, if your headaches are severe, if they significantly impact your quality of life, or if your doctor suspects a more complex headache disorder.
Q6: Can lifestyle changes genuinely help with a daily headache?
Absolutely. Lifestyle adjustments are a cornerstone of managing daily headache. Consistent sleep, regular exercise, adequate hydration, a balanced diet, caffeine moderation, stress management techniques, and identifying personal triggers can significantly reduce headache frequency and severity.
For more information, visit: National Institute of Neurological Disorders and Stroke











Post Comment